Gastric sleeve surgery is a prominent bariatric procedure involving the removal of a large portion of the stomach, significantly reducing its size to curb appetite and promote weight loss. This method is gaining traction globally for its effectiveness in treating obesity-related health issues. The following guide provides insights into its benefits, procedure details, and frequently asked questions to equip potential patients with comprehensive knowledge.

Gastric sleeve surgery, also known as sleeve gastrectomy, is a transformative weight-loss procedure increasingly sought after by individuals struggling with obesity. It involves surgically removing a substantial portion of the stomach, resulting in a sleeve-like structure that significantly limits food intake and, consequently, caloric consumption. The rise in obesity rates globally has made surgical interventions an essential option for many, leading to increased interest in procedures like the gastric sleeve.
Gastric sleeve surgery operates on a simple principle: reducing the stomach's capacity leads to reduced food intake and subsequent weight loss. This method not only limits the amount of food one can consume but also influences hormonal balances, notably decreasing hunger-inducing hormones. A key hormone affected by this procedure is ghrelin, which is primarily produced in the stomach; its reduction contributes to lower appetite levels post-surgery.
The surgery is generally performed laparoscopically under general anesthesia, minimizing incision sizes and promoting faster recovery. Laparoscopic surgery involves small incisions rather than a large opening, which helps reduce pain, scarring, and recovery time compared to open surgical methods. During the operation, roughly 75-85% of the stomach is removed, leaving a tubular pouch, or "sleeve," which dramatically reduces the size of the stomach. The surgeon typically stitches the remaining stomach at the site of the resection to create this new shape.
Before undergoing gastric sleeve surgery, patients typically go through a comprehensive evaluation, including consultations with physicians, nutritionists, and surgeons to assess their overall health and readiness for the procedure. This pre-operative phase involves understanding the surgery, setting realistic weight loss goals, and developing a pre-operative diet plan. Often, patients are recommended to lose a certain amount of weight before surgery to decrease liver size and optimize surgical conditions, enhancing recovery post-operation.
| Procedure Type | Description | Pros | Cons |
|---|---|---|---|
| Gastric Sleeve | Removes a portion of the stomach. | Reduced appetite, quick recovery. | Irreversible, risk of complications. |
| Gastric Bypass | Alters stomach and intestines. | Significant weight loss. | More complex, malabsorption issues. |
| Adjustable Band | Band placed around the stomach. | Adjustable, reversible. | Less weight loss, frequent adjustments. |
| Biliopancreatic Diversion | Removes part of the stomach and bypasses significant portions of the small intestine. | Greater weight loss, improved metabolic conditions. | Higher risk of deficiencies and complex recovery. |
As with any major surgery, gastric sleeve procedures come with risks including bleeding, infection, and potential leaks from the stomach. Good considerations include nutritional deficiencies and the need for lifestyle adjustments to maintain weight loss. Patients may experience complications such as strictures (narrowing of the stomach pouch), hernias, and gastroesophageal reflux disease (GERD). Regular follow-up visits with healthcare providers will be essential to monitor recovery and nutritional health.
While many patients achieve significant weight loss, maintaining this weight loss requires long-term commitment to healthy eating and physical activity. Medical professionals often recommend regular follow-ups to monitor weight, nutritional levels, and overall health. A nutritionist may assist patients in developing meal plans that ensure they meet their dietary needs despite the reduced stomach size. Additionally, community support groups can be invaluable, providing motivation and a sense of accountability.
Recovery typically spans a few weeks, with dietary restrictions including a liquid diet initially, gradually progressing to soft and then solid foods. Post-operative care emphasizes an understanding of portion control and the types of foods that are more easily digestible. Patients are advised to eat slowly, chew food thoroughly, and practice mindful eating to maximize their success.
Initially, the diet consists of clear liquids to allow the stomach to heal, and as healing progresses, patients can move to pureed foods and eventually to soft foods. Nutritional inclusivity becomes essential, focusing on high-protein, low-sugar, and low-fat diets, supplemented with vitamins and minerals as necessary. Since the surgery alters the stomach's ability to absorb nutrients, patients often need to take vitamin supplements for life, addressing potential deficiencies in vitamin B12, iron, calcium, and vitamin D.
Alongside dietary changes, incorporating regular physical activity is critical for long-term weight management. After surgery, patients can gradually reintroduce physical activities, typically starting with walking and slowly progressing to more intense workouts as they feel comfortable. Engaging in regular exercise helps not only in weight loss but also in improving mood, enhancing cardiovascular health, and fostering overall well-being.
The cost of gastric sleeve surgery can vary widely depending on geographic locations, healthcare providers, and facility types. In the United States, the average cost ranges from $15,000 to $25,000. Patients are encouraged to explore options that balance affordability with quality care. Many insurance plans might cover part or all of the procedure, depending on the patient's obesity classification, medical history, and completion of necessary pre-operative guidelines.
Patients considering gastric sleeve surgery should not only take into account the initial surgery costs but also potential long-term expenses, including follow-up consultations, dietary supplements, and possibly additional treatments for complications. Consulting with financial advisors or the hospital’s billing department can provide clarity about payment options, insurance coverage, and financing plans available. Budgeting for both direct and indirect costs associated with the surgery will help patients prepare effectively.
A robust support system can significantly affect the success of the gastric sleeve journey. Patients might find comfort in connecting with others who have undergone similar surgical procedures through local or online support groups. These groups offer a space to share experiences, discuss challenges, celebrate successes, and maintain motivation. Many clinics and hospitals provide resources such as counseling services, nutritional workshops, and exercise classes, paving the way for a supportive environment post-surgery.
Gastric sleeve surgery presents a viable option for those seeking a sustainable solution to obesity. While the surgery offers significant health benefits, individuals must weigh the risks, costs, and necessary lifestyle changes when considering this procedure. The journey post-surgery demands dedication and adjustment, requiring both physical and emotional resilience. As with any medical decision, consulting with healthcare professionals is crucial in making informed, personalized choices, ensuring that the decision taken is not only right for the body but also aligns with personal health goals and life aspirations.
To further understand the impact of gastric sleeve surgery, it is vital to explore real-life success stories from individuals who have undergone the procedure. Many find tremendous transformation in their lives, not just in weight loss but also in their confidence, health, and overall outlook. Sharing these stories helps illustrate the journey, having both its challenges and triumphs.
Emma, a 34-year-old mother of two, struggled with obesity for most of her life. After numerous unsuccessful attempts at dieting and exercise, she considered gastric sleeve surgery. Post-surgery, Emma lost over 100 lbs within a year and has significantly improved her health metrics, including her blood pressure and cholesterol levels. The surgery taught her the importance of nutrition, leading her to become an advocate for healthy eating in her community. Emma credits the surgical team and her support group for her ongoing success, emphasizing that surgery was just the first step in a much larger journey.
David, a 42-year-old man who dealt with obesity-induced diabetes, found gastric sleeve surgery to be life-saving. After the procedure, he adopted a rigorous exercise regimen and lost nearly 80 lbs within 18 months, achieving remission from diabetes. David attends a weekly fitness class and has become a motivational speaker in his local area, encouraging others to embrace change and seek help when needed. His story exemplifies the broader potential of gastric sleeve surgery, showcasing the importance of taking action towards health and wellness.
For Maria, 29, the decision to have gastric sleeve surgery was not a light hearted one. Growing up, she faced bullying due to her weight, leading her to develop anxiety and depression. Following her successful surgery, Maria embarked on a journey of self-discovery alongside her physical transformation. She lost over 90 lbs and found joy in activities she previously avoided, such as hiking and dancing. Maria’s journey also included mental health support, which she highlights as crucial to her transformation. Now, she advocates for mental health awareness in conjunction with discussions around obesity and weight loss surgery.
These narratives illustrate the profound impact gastric sleeve surgery can have on an individual's life. While not every story will unfold in the same way, they highlight the collective power of determination, medical intervention, and community support. The path to weight loss and enhanced health is often multifaceted, demanding an approach that includes psychological, nutritional, and physical elements. It's essential for each patient to find their own story amidst the shared experiences, allowing for hope and inspiration as they navigate their transformation journey.
Explore the Tranquil Bliss of Idyllic Rural Retreats

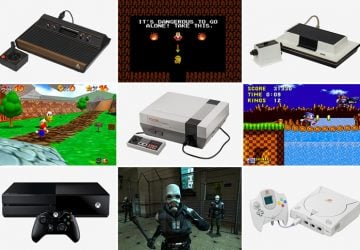
Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!
Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
