Gastric Sleeve Surgery is a popular weight-loss surgical procedure that involves reducing the size of the stomach to help individuals eat less food and lose weight. Originated to combat severe obesity, it has evolved into a staple in bariatric surgery, globally recognized for its effectiveness and safety. This article explores the intricacies of Gastric Sleeve, its benefits, eligibility, and considerations for potential patients.
Gastric Sleeve Surgery, also known as sleeve gastrectomy, is a type of bariatric surgery designed primarily for significant weight loss. This increasingly popular procedure involves the removal of a large portion of the stomach, typically around 75-80%. The surgery results in a tube or "sleeve" shaped stomach that is significantly smaller than its original size. By limiting the volume of food that can be consumed, it plays a crucial role in helping individuals manage their obesity and weight-related health issues effectively.
Beyond merely reducing stomach size, Gastric Sleeve Surgery also alters hormonal levels in the body which regulate hunger and satiety. This physiological change further assists in weight loss by reducing appetite and increasing the sensation of fullness. The surgery positions itself as an effective solution for those struggling with obesity, particularly when other methods of weight loss—like diet and exercise—have failed.
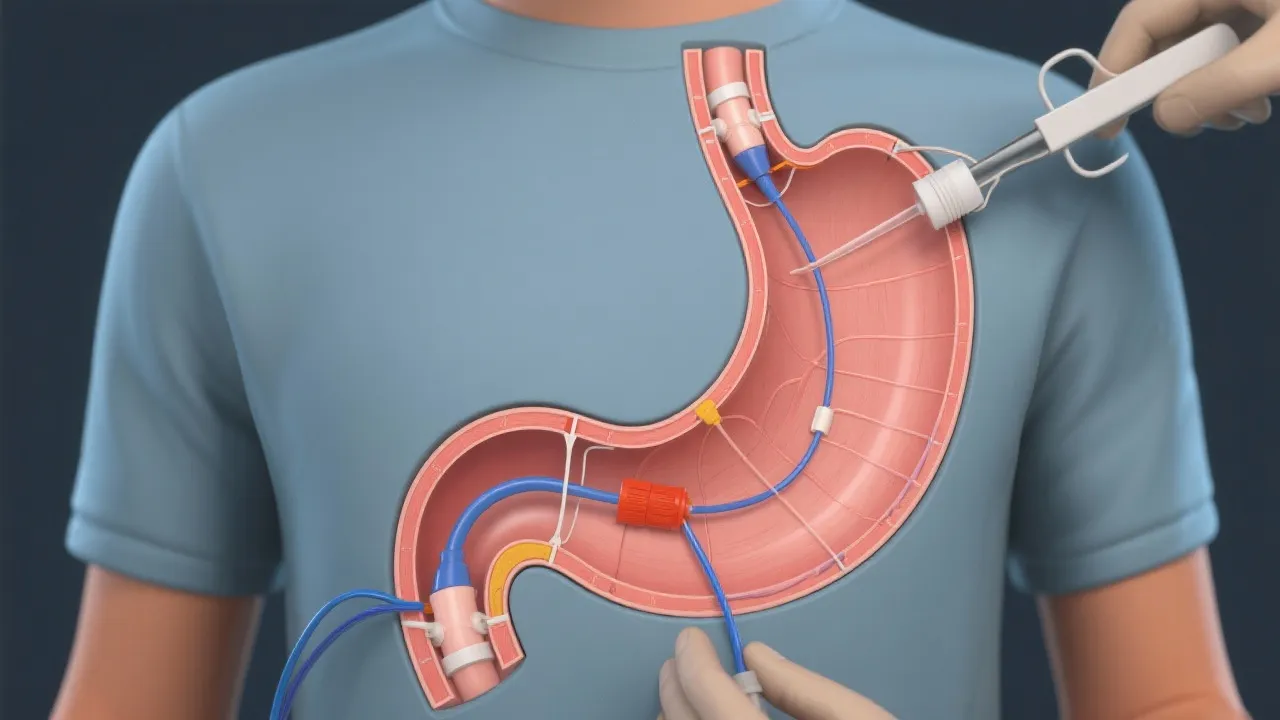
The Gastric Sleeve procedure is typically performed laparoscopically, which is a minimally invasive surgical technique involving small incisions in the abdomen. During this method, specialized surgical instruments and a camera (laparoscope) are utilized to guide the surgery, allowing for reduced patient recovery time compared to traditional open surgery. Once the surgical team determines the correct placement, the surgeon skillfully removes the designated portion of the stomach, which is then stapled and reshaped into a slender sleeve.
The entire process usually takes one to two hours, with patients typically staying in the hospital for two to three days post-surgery for observation and recovery. During the initial phase of recovery, patients may experience discomfort, but this can generally be managed with prescribed medications. It is essential for patients to follow their surgical team's guidelines closely to promote healing and avoid complications. After returning home, most individuals are advised to incorporate walking and light physical activity into their daily routines to further aid in recovery.
The primary advantage of Gastric Sleeve Surgery is its significant potential for weight loss. Studies show that many patients report losing between 50-70% of their excess body weight within the first two years following the surgery, making it one of the most effective weight-loss solutions available. Additionally, this procedure can lead to resolution or improvement of several obesity-related conditions, such as chronic type 2 diabetes, high blood pressure, joint pain, and obstructive sleep apnea. The reduction in stomach size not only curtails food intake but also affects appetite-regulating hormones, creating an enhanced feeling of fullness which encourages healthier eating patterns and aids in long-term weight management.
Moreover, many patients experience improvements in their overall quality of life post-surgery. Patients often report increased energy levels, improved mobility, and enhanced mental health as a result of their weight loss. The psychological effects can be profound, as many individuals report increased self-esteem and improved relationships with friends and family following a successful weight-loss journey. This holistic improvement reflects the comprehensive advantages that Gastric Sleeve Surgery can bring beyond the scales, significantly impacting a patient's life overall.
Candidates for Gastric Sleeve Surgery are typically individuals with a body mass index (BMI) of 40 or higher, or those with a BMI of 35 or higher who also suffer from serious obesity-related health conditions. Prospective patients are required to undergo a comprehensive evaluation process which often includes dietary counseling, physical examinations, and sometimes psychological assessments. The psychological evaluation is particularly significant, as it helps identify any underlying mental health issues that may affect a patient's ability to maintain a successful post-surgical lifestyle.
Once a candidate is deemed suitable for the surgery, they are often required to participate in a pre-surgery weight loss program. This can help shrink the liver and prepare the abdominal area for surgery, ultimately enhancing surgical safety and efficacy. These preparations can also help patients begin their transition into a healthier lifestyle, making them more equipped for the changes that accompany life post-surgery. It's essential for individuals to have realistic expectations about what the procedure entails and to be committed not just to the surgery itself, but to the lifestyle and dietary changes that will follow.
As with any surgical procedure, Gastric Sleeve Surgery carries potential risks that patients need to be fully aware of. Some of these risks encompass infections, excessive bleeding, and complications related to anesthesia. Although rare, some patients may experience leaks from the newly created sleeve, which can necessitate further surgical intervention. Another important post-operative consideration is the potential for nutrient absorption issues. Due to the reduced size of the stomach and changes to the digestive system, lifelong vitamin and mineral supplementation is required to prevent deficiencies.
One aspect that cannot be overlooked is the psychological adjustment that follows surgery. The drastic change in body size and food habits can result in emotional challenges, and patients must be prepared for this journey. Support groups, counseling, or nutritional therapy may be beneficial in helping patients navigate the emotional and psychological adjustments that accompany such a significant lifestyle change. It's crucial for individuals to weigh these risks against the benefits and engage in thorough discussions with their healthcare providers to ensure a well-informed decision regarding the surgery.
| Aspect | Gastric Sleeve | Gastric Bypass |
|---|---|---|
| Stomach Size Reduction | 75-80% | Significant along with rerouting the small intestine |
| Procedure Time | 1-2 hours | 2-4 hours |
| Typical Hospital Stay | 2-3 days | 3-5 days |
| Recovery Time | 2-4 weeks | 4-6 weeks |
| Weight Loss | 50-70% excess weight | 60-80% excess weight |
| Nutritional Deficiency Risk | Moderate, requires vitamins | Higher, requires stricter monitoring |
| Long-term Maintenance | Requires lifestyle changes, moderation in eating habits | Requires strict dietary adherence due to malabsorption |
Before undergoing Gastric Sleeve Surgery, patients typically undergo several preparatory steps that are designed to ensure the safest and most effective outcome. These steps may include:
Recovery from Gastric Sleeve Surgery involves a gradual transition from a liquid diet to a solid food diet over several weeks. Patients are encouraged to take small steps towards incorporation of more varied food groups in a timely but measured manner. The progression typically starts with clear liquids, then moves on to full liquids, pureed foods, and eventually solid foods. Patients are encouraged to engage in light physical activity early on, gradually increasing intensity as they begin to feel stronger. Most individuals return to their regular routines within four to six weeks post-surgery, allowing for sufficient healing time and adaptation to the new eating patterns.
Yes, Gastric Sleeve Surgery is considered a good procedure for individuals who meet the eligibility criteria and are struggling with obesity. It has been shown to have significant long-term effects on weight loss and the reduction of obesity-related conditions. However, as with any surgical intervention, outcomes can vary by individual. In rare cases, complications may arise, or patients may not achieve the expected weight loss. Thus, ongoing follow-up care and commitment to lifestyle changes are critical components of post-surgical success.
Yes, the stomach can stretch over time after Gastric Sleeve Surgery if individuals do not adhere to the dietary recommendations provided by healthcare professionals. Inconsistent eating habits, high-calorie foods, and lack of portion control can lead to the stomach gradually increasing in size. Good long-term success after surgery not only depends on physical changes but also heavily relies on lifestyle modifications and supportive measures that reinforce adherence to a healthy diet and regular physical activity.
Post-surgery, patients must follow a structured eating plan that evolves over time. Initially, the diet will be limited to liquids, progressing to pureed foods, then soft foods, and eventually solid foods. Patients must focus on protein-rich foods while avoiding high-sugar and high-fat items. Increased protein intake helps with healing and preserves lean muscle mass while losing weight. It’s advisable to eat small meals, approximately five to six times a day, and stay hydrated, aiming for at least 64 ounces of water daily. Most importantly, individuals should chew their food thoroughly to facilitate digestion and prevent discomfort.
While many patients experience significant weight loss within the first year or two after Gastric Sleeve Surgery, maintaining that weight loss depends on the individual's commitment to lifestyle changes. Following the initial rapid weight loss phase, the pace may slow but continued adherence to healthy dietary practices and regular physical activity is crucial for long-term success. Patients who incorporate lifestyle changes into their daily routines often maintain their weight loss for many years post-surgery. Regular follow-ups with a healthcare team can provide support and resources to help keep patients on track.
Pregnancy is possible after Gastric Sleeve Surgery; however, it is essential for women to allow adequate time for recovery and stabilization of their weight before attempting conception. Many providers recommend that patients wait at least 18-24 months post-surgery before becoming pregnant to ensure that they have achieved significant weight loss and are accustomed to their new dietary habits. Proper nutritional intake during surgery recovery can affect pregnancy health, and ongoing prenatal care is particularly important to support both the mother and the baby during pregnancy.
Following Gastric Sleeve Surgery, numerous support avenues are available to assist patients in navigating their weight loss journey. Many bariatric programs host support groups or provide access to dietitians and mental health professionals specializing in obesity and weight loss. These resources offer opportunities to connect with others who are undergoing similar experiences, share success stories, and discuss challenges encountered along the way. Additionally, some patients may benefit from individual counseling to address emotional factors that affect eating behaviors, while mobile applications and online communities can provide ongoing virtual support.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
