Atopic dermatitis, a chronic inflammatory skin condition, is characterized by symptoms such as dry, itchy skin, and eczema. This article explores the condition's complexities, focusing on visual presentations to help individuals and clinicians recognize and manage the condition effectively. By examining these visual cues, our aim is to provide a deeper understanding of atopic dermatitis and strategies for its management.
Atopic dermatitis, commonly referred to as eczema, is more than just a skin condition; it’s a chronic inflammatory disease that significantly affects millions of people globally. Atopic dermatitis is marked by dry, itchy skin and can manifest in various ways, resulting in red, inflamed patches that can be uncomfortable for those affected. The condition is particularly prevalent in children, although it can occur at any age. As such, understanding its characteristics is essential for effective management and improving the quality of life for individuals living with this condition. This article delves into the visual aspects of atopic dermatitis, providing an extensive guide to understanding its presentations, implications, and treatment options.
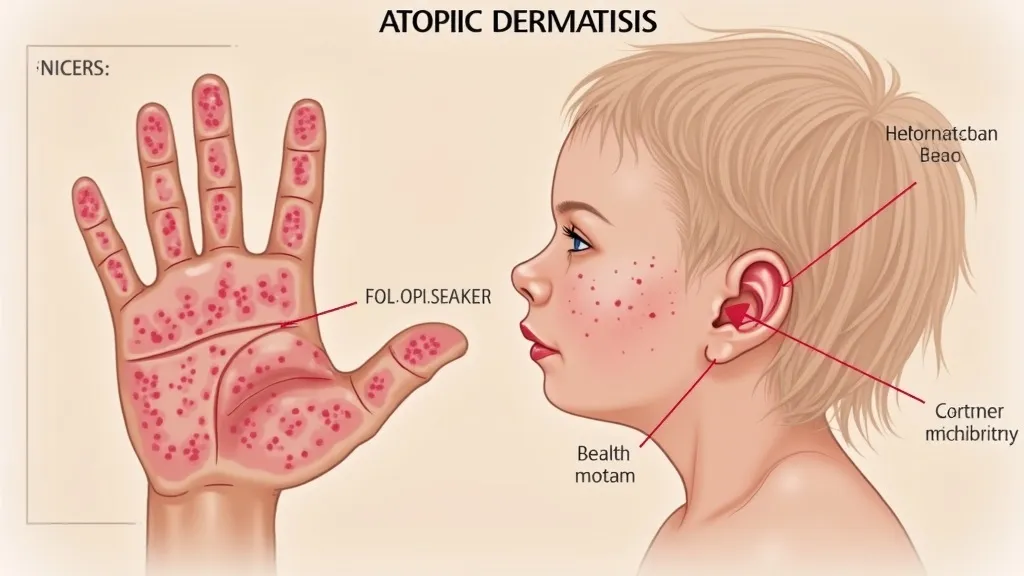
Atopic dermatitis presents a diverse range of symptoms that can vary widely among individuals, and understanding these visual variations is crucial for accurate diagnosis and effective treatment. Atopic dermatitis pictures often illustrate dry, scaly patches of skin that may appear cracked or leathery. Other noteworthy characteristics include inflammation and redness, which can vary in intensity. In some cases, affected areas can become swollen; intense scratching can lead to further complications like skin infections or flare-ups. The condition typically follows a relapsing-remitting course, meaning that individuals can experience periods of exacerbation followed by phases of remission.
Several factors contribute to the appearance and severity of atopic dermatitis symptoms. Genetic predisposition plays a significant role, with a higher incidence observed among individuals with a family history of atopy, which includes conditions like asthma and hay fever. Environmental triggers, ranging from allergens such as dust mites, pollen, and pet dander to irritants like soaps, detergents, and even certain fabrics, can exacerbate symptoms. Additionally, climatic conditions, such as cold, dry air or high humidity, can affect the skin’s condition. Emotional stress is another critical factor, as it can lead to increased itching and scratching, creating a vicious cycle of worsening symptoms and elevated stress levels. Thus, it becomes essential for individuals to identify and avoid these triggers to mitigate flare-ups and maintain optimal skin health.
Although medical history and clinical evaluation through a physical examination are vital for diagnosing atopic dermatitis, visual assessment of the affected skin is equally important. Clinicians rely heavily on visual clues to differentiate atopic dermatitis from other skin conditions such as psoriasis, contact dermatitis, and seborrheic dermatitis. A detailed analysis of the distribution, pattern, and morphology of skin lesions is crucial in establishing a correct diagnosis. For instance, atopic dermatitis is frequently localized to the creases of the extremities (like the elbows and knees) in adults while presenting differently in infants, often appearing on the face and scalp. Observations like the presence of oozing, crusting, or signs of bacterial infection can also assist dermatologists in making an informed evaluation.
| Condition | Visual Indicators | Distinguishing Features |
|---|---|---|
| Atopic Dermatitis | Red, inflamed, dry patches | Itchy; surfaces may appear cracked and leathery |
| Psoriasis | Silvery scales, well-defined borders | Thicker scales, less itching compared to eczema; more often found on the scalp, elbows, and knees |
| Contact Dermatitis | Blisters, weeping sores | Caused by direct contact with irritants/allergens; inflammation localized to affected areas |
| Seborrheic Dermatitis | Greasy, yellowish scales on a red base | Typically occurs in areas with high oil production, such as the scalp and face |
Effectively managing atopic dermatitis involves a comprehensive approach combining lifestyle changes, diligent skincare routines, and medical treatments tailored to individual needs. Dermatologists often recommend moisturizers aimed at restoring the skin barrier, emphasizing the importance of regular and liberal application of emollients. These moisturizers help trap moisture in the skin, preventing dryness and reducing the frequency of flare-ups.
Topical corticosteroids are a common first-line treatment to reduce inflammation and alleviate itching during flare-ups. While they are effective, long-term use may lead to side effects, prompting healthcare providers to consider alternatives in some cases. Newer classes of topical medications, such as calcineurin inhibitors like tacrolimus and pimecrolimus, are often prescribed for sensitive areas of skin (like the face) and are preferred due to their reduced risk of side effects compared to corticosteroids.
For more severe cases that do not respond adequately to topical treatments, systemic medications such as oral corticosteroids or immunosuppressants may be necessary; however, these are typically reserved for extreme cases due to potential side effects. In recent years, biological therapies, such as dupilumab (Dupixent), have shown promise for patients with moderate to severe atopic dermatitis. These treatments work by targeting specific pathways in the immune system, demonstrating significant efficacy in improving skin symptoms and leading to near-complete clearance in many patients.
In addition to conventional treatments, many individuals find relief through complementary therapies, which may include natural remedies and lifestyle adjustments. For example, adding omega-3 fatty acids through diet or supplementation has been studied for its anti-inflammatory properties, and some people report improvements with evening primrose oil or fish oil. Mindfulness practices, such as yoga and meditation, can also be beneficial in managing the stress that may trigger flare-ups. Furthermore, it’s essential for those with atopic dermatitis to adapt their skincare routines — this includes avoiding known irritants and using soap-free cleansers and gentle skincare products. Regular lukewarm baths followed by the immediate application of moisturizer can help maintain skin hydration.
Managing atopic dermatitis can be emotionally and physically taxing. Emotional support plays a crucial role in coping with the daily challenges of living with this chronic condition. Support groups, whether in-person or online, provide a space for individuals to share their experiences and coping strategies. Additionally, many organizations dedicated to eczema and skin health offer valuable resources, including educational materials, treatment guidelines, and forums for connection. Engaging with healthcare providers for ongoing education and support can empower individuals to take control of their skin health and navigate the ups and downs of living with atopic dermatitis more effectively.
Understanding and managing atopic dermatitis requires a comprehensive approach focused on identifying individual symptoms and triggers. Through visual analysis and a tailored treatment plan crafted in collaboration with healthcare providers, managing this persistent condition becomes feasible. Advances in treatments, ranging from topical medications to novel biological therapies, have significantly improved the outlook for many individuals with eczema. Support systems, education, and a proactive approach to skincare can lead to a richer, more fulfilling life for those affected by this condition.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
