Non-alcoholic fatty liver disease (NAFLD) progressing to hepatocellular carcinoma (HCC) is a significant health concern, impacting persons worldwide. NAFLD Related HCC represents a challenging area within hepatology, requiring a multifaceted approach to treatment and management. This comprehensive guide explores the latest insights, interventions, and strategies to address this issue, emphasizing early detection and lifestyle changes.
In recent years, Non-alcoholic fatty liver disease (NAFLD) has emerged as a prevalent liver condition characterized by excessive fat accumulation in the liver of individuals who consume little or no alcohol. Globally, NAFLD has affected an estimated 25% of the population, and its prevalence is on the rise, largely attributed to unhealthy lifestyle choices, such as poor dietary habits and lack of physical activity. When left unchecked, NAFLD can advance to non-alcoholic steatohepatitis (NASH), which is a more severe form of the disease marked by inflammation and liver cell damage. NASH can further lead to hepatocellular carcinoma (HCC), a primary form of liver cancer. Understanding NAFLD-related HCC is crucial due to the increasing global incidence and significant healthcare implications associated with both conditions. With the burden of NAFLD and HCC expected to rise, public health efforts must prioritize this issue to avert a looming health crisis.
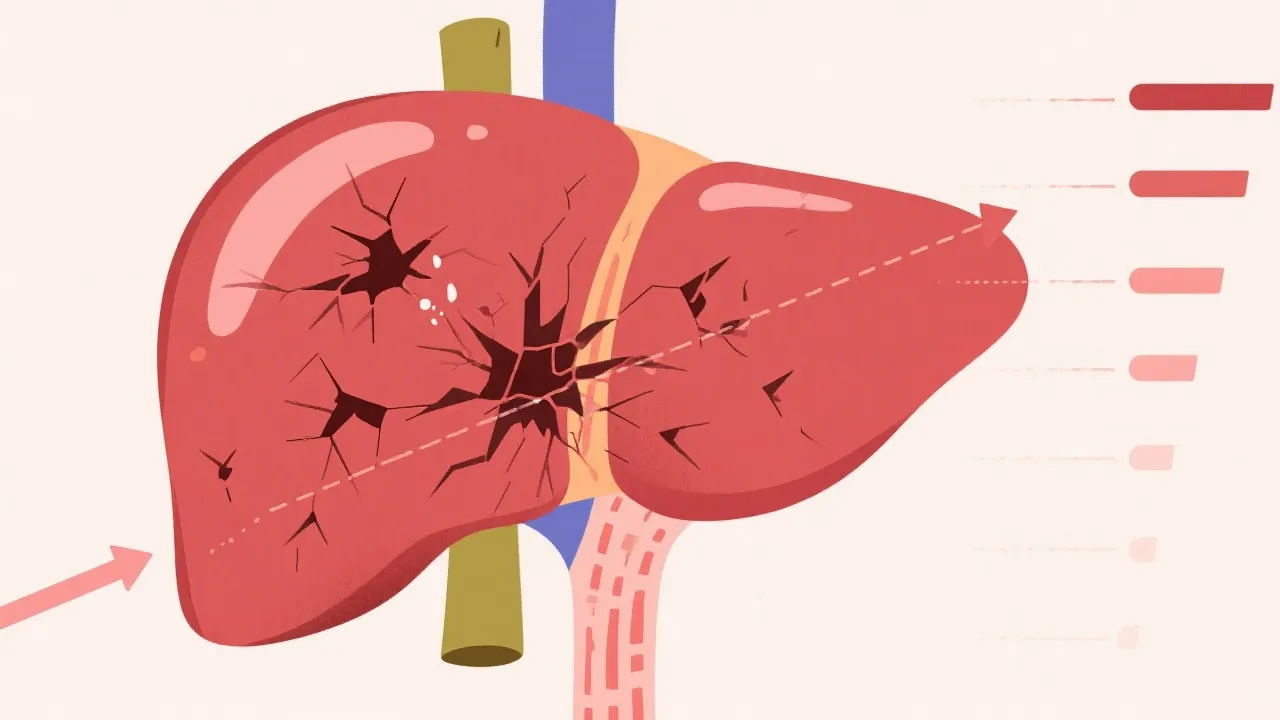
The transition from NAFLD to HCC involves a complex interplay of metabolic, genetic, and environmental factors. Initially, benign fat accumulation in the liver can trigger inflammation and fibrosis, both of which are characteristic of NASH. This ongoing inflammatory response leads to a cascade of cellular events that can result in cellular injury, apoptosis, and the activation of fibroblasts—cells that produce collagen and promote scarring within the liver tissue. This accumulation of scar tissue replaces healthy liver cells, leading to cirrhosis, which is a known precursor to HCC. Moreover, persistent liver damage causes genomic instability and malignant transformation of hepatocytes, culminating in liver cancer. This pathophysiological cascade underscores the importance of early intervention to prevent the progression of NAFLD to malignant stages, emphasizing the need for enhanced understanding and awareness of these conditions.
Key risk factors for NAFLD-related HCC include obesity, type 2 diabetes, and metabolic syndrome. Individuals with a higher body mass index (BMI) are particularly susceptible as excess body fat contributes to liver inflammation and damage. Furthermore, the presence of type 2 diabetes often exacerbates these conditions due to the insulin resistance associated with both disorders. Genetic predispositions also play a role, with certain polymorphisms, such as those affecting the PNPLA3, TM6SF2, and GCKR genes, increasing susceptibility to liver disease progression. These genetic factors complicate risk stratification and highlight the importance of personalized medicine in managing NAFLD and its complications.
Early detection of NAFLD and its progression is paramount, as interventions at this stage can significantly alter the disease trajectory. Advances in imaging techniques and biomarker research have facilitated improved surveillance strategies. Routine liver function tests, imaging modalities like ultrasound, and the evaluation of specific biomarkers, such as liver stiffness measurement and fibrosis scores, are integral for timely diagnosis and intervention. Emerging non-invasive biomarkers are being studied to provide further insights into liver histology without the need for biopsy, which remains the gold standard but is often limited by its invasiveness and associated complications.
Lifestyle changes are foundational in managing NAFLD and preventing its progression. A healthy diet low in saturated fats, sugars, and refined carbohydrates can significantly impact liver health. A Mediterranean diet, which emphasizes whole grains, fruits, vegetables, legumes, and healthy fats, has shown promising results in improving liver histology and reducing fatty liver content. Regular physical activity, encompassing both aerobic exercises and resistance training, is also proven to be effective in reducing liver fat and inflammation. Weight loss remains one of the most effective interventions for NAFLD, with studies suggesting that a 5-10% reduction in body weight can lead to significant improvements in liver health.
Pharmacological treatments targeting insulin resistance, dyslipidemia, and fibrosis are also being explored. Medications such as metformin, pioglitazone, and vitamin E have been utilized with varying outcomes in clinical studies. Emerging therapies, including peroxisome proliferator-activated receptor (PPAR) agonists and fibroblast growth factor 21 (FGF21) analogs, show promise in clinical trials, with substances like obeticholic acid and elafibranor receiving special attention for their potential to reverse liver damage and reduce the risk of cancer development.
Furthermore, managing co-morbidities such as hypertension and hyperlipidemia is vital in the comprehensive treatment of patients with NAFLD. Given the complexities of metabolic syndrome, a multidisciplinary approach involving nutritionists, physical therapists, hepatologists, and endocrinologists is often necessary to optimize patient outcomes.
The treatment of NAFLD-related HCC requires a comprehensive, multidisciplinary approach. Traditional treatments, such as surgical resection and liver transplantation, remain critical for eligible patients. The decision to perform a resection depends on the tumor's size, location, and the overall liver function. Liver transplantation offers a curative option for patients with advanced cirrhosis and HCC, considering suitable donor availability and strict selection criteria.
However, advancements in locoregional therapies, including radiofrequency ablation (RFA) and transarterial chemoembolization (TACE), have expanded options for those with unresectable tumors. RFA utilizes heat to destroy cancer cells, while TACE delivers chemotherapy directly to the tumor, minimizing systemic exposure. These localized approaches provide significant symptomatic relief and are effective in prolonging survival rates in selected patient populations.
Systemic therapies, notably immune checkpoint inhibitors, have revolutionized the treatment landscape in the past decade. The introduction of agents like nivolumab and pembrolizumab offers new hope for prolonged survival by enhancing the body’s immune response against cancer cells. Additionally, multi-kinase inhibitors such as sorafenib and lenvatinib have been pivotal in the treatment of advanced HCC, providing more options for patients who have progressed on prior therapies. Ongoing clinical trials are exploring novel combinations and sequencing of therapies to optimize patient outcomes further.
Moreover, the role of personalized medicine is increasingly recognized in the management of HCC. Genetic profiling and molecular characterization can help identify targets for therapy, tailoring approaches that maximize efficacy and minimize toxicity.
The rising prevalence of NAFLD and its potential progression to HCC pose significant challenges to healthcare systems worldwide. The economic burden is substantial, encompassing not only the costs of treatment but also the indirect costs associated with loss of productivity and quality of life. As NAFLD becomes a leading cause of liver disease-related morbidity and mortality, health systems must adapt to manage this demographic shift effectively. This requires investment in public health initiatives focusing on awareness, prevention, and early intervention to mitigate these impacts.
Moreover, the burden of NAFLD and HCC is not evenly distributed, with socio-economic disparities influencing prevalence and outcomes. Access to healthcare, education regarding lifestyle choices, and availability of resources significantly affect the disease trajectory within populations. Targeted public health campaigns and community-based interventions tailored to specific populations can improve awareness and reduce the incidence of NAFLD-related HCC.
Implementing preventive strategies such as health education, promoting healthy dietary habits, and encouraging regular physical activity are crucial in addressing the growing burden of liver diseases. Efforts should also focus on screening high-risk populations, including those with obesity, diabetes, and metabolic syndrome, to facilitate early detection of liver abnormalities. Policymakers must recognize the importance of addressing NAFLD and HCC as pivotal components of liver health initiatives while promoting research and development of innovative therapeutic strategies.
| Strategy | Description |
|---|---|
| Lifestyle Modification | Diet changes, exercise, and weight management to reduce liver fat. |
| Pharmacological Treatment | Emerging drugs targeting metabolic pathways and fibrosis. |
| Surgical Intervention | Resection or transplantation for eligible HCC patients. |
| Locoregional and Systemic Therapies | Innovations like immune checkpoint inhibitors and ablation techniques. |
Receiving a diagnosis of NAFLD or HCC can significantly impact an individual’s mental and emotional well-being. Patients may experience anxiety, depression, and fear related to their health condition. It is crucial for healthcare providers to address the psychological aspects of living with chronic liver disease by offering supportive resources such as counseling, support groups, and mental health services. Additionally, fostering effective communication between patients and healthcare providers can facilitate shared decision-making and enhance patient engagement in their care.
Moreover, members of the community can play an essential role in supporting individuals with NAFLD and HCC. Education initiatives targeted at increasing public awareness of liver health can empower individuals to make informed lifestyle choices and promote healthy behaviors. Patients can benefit from community programs focusing on nutrition, fitness, and disease self-management, equipping them with the tools necessary to better manage their health.
Follow-up care is important for all liver disease patients as it helps monitor disease progression, manage complications, and adjust treatment plans accordingly. Regular check-ups with healthcare professionals are essential for ensuring optimal management and addressing new or worsening symptoms in a timely manner.
The understanding and management of NAFLD-related HCC are crucial for addressing this growing health issue. By emphasizing the importance of early detection, lifestyle intervention, and innovative treatments, healthcare professionals can significantly impact outcomes for those at risk. Leveraging multidisciplinary approaches, continuous education, and patient-centered strategies will be critical in tackling these complex conditions effectively. With the world facing a rising tide of liver-related diseases, it is more important than ever to unite efforts across public health, clinical practice, and research to confront this emerging epidemic.
Cultivating a comprehensive understanding of NAFLD and HCC, coupled with effective management strategies, will play an indispensable role in mitigating the effects of these conditions on individual and public health. Continuous investment in research and support for patients, alongside collaborative public health efforts, will significantly reshape the landscape of liver disease management in the coming years.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
