This article delves into the transformative impact of Pre-Exposure Prophylaxis (PrEP) on HIV prevention strategies. PrEP has become a cornerstone in reducing HIV transmission risk among high-risk populations. For readers seeking to understand PrEP's role in the global fight against HIV, this piece provides in-depth analysis, current research, and expert insights into the promising future of this prevention method.
Pre-Exposure Prophylaxis, commonly known as PrEP, represents a significant advancement in HIV prevention efforts. This strategy, which involves the use of antiretroviral medication by HIV-negative individuals to prevent infection, has emerged as a crucial component in the global battle against HIV. As the prevalence of HIV remains a significant public health issue worldwide, strategies like PrEP offer promising hope in reducing transmission risk, particularly among high-risk groups.
With an estimated 37.7 million people living with HIV across the globe, according to the World Health Organization (WHO), the quest for effective prevention methods has never been more urgent. PrEP is not just a preventive measure but a transformative approach that allows individuals to take an active role in their sexual health. This empowerment is especially important in regions heavily impacted by the epidemic, where traditional prevention methods may not be sufficient or accessible.
PrEP involves the daily intake of a combination of antiretroviral drugs to prevent HIV infection in individuals who are HIV-negative but at high risk. The very common PrEP regimen includes the drugs tenofovir and emtricitabine, which work to inhibit the virus’s lifecycle within the body. By maintaining therapeutic drug levels in the bloodstream, PrEP significantly reduces the risk of HIV establishing an infection, thus serving as an effective preventive measure.
The mechanism of PrEP is grounded in pharmacokinetics; the medications are designed to work effectively when taken consistently. When the HIV virus enters the bloodstream, it needs to bind to CD4 cells, a type of white blood cell that plays an essential role in immune response. The antiretroviral components of PrEP inhibit the reverse transcriptase enzyme, thereby blocking the virus from replicating and spreading within the body. Thus, PrEP not only prevents the establishment of infection but also plays a role in reducing the viral load among HIV-positive individuals who may be unaware of their status.
Numerous studies have demonstrated the effectiveness of PrEP in preventing HIV transmission. According to a study published in the New England Journal of Medicine, consistent adherence to PrEP can reduce the risk of HIV infection by more than 90% in individuals who take the medication as prescribed. This underscores the importance of adherence to the daily regimen to harness its full protective benefits.
A meta-analysis evaluating various PrEP studies indicates that different demographic groups may experience varying levels of effectiveness. Targeted populations, including men who have sex with men, transgender individuals, and people who inject drugs, have seen substantial reductions in new HIV infections when utilizing PrEP. Furthermore, even sporadic use of PrEP can provide some level of protection; however, the best outcomes are observed with consistent daily ingestion of the medication. This nuanced understanding is critical as healthcare providers work with patients to develop personalized prevention plans.
Despite its effectiveness, the implementation of PrEP faces several challenges. One significant concern is adherence, as its effectiveness diminishes with irregular use. Factors influencing adherence include forgetfulness, stigma, and lack of immediate access to healthcare resources. In some cases, individuals may experience anxiety related to taking medications daily, leading them to forego the treatment entirely.
Additionally, there are issues related to accessibility, affordability, and awareness, particularly in low-income regions and marginalized communities. Stigma associated with HIV and PrEP use can also hinder its wider adoption. Many individuals feel embarrassed or ashamed to seek out information about PrEP or discuss their concerns with healthcare providers. Misconceptions about who can benefit from PrEP perpetuate stigma, particularly within communities that harbor deeply entrenched biases about HIV transmission.
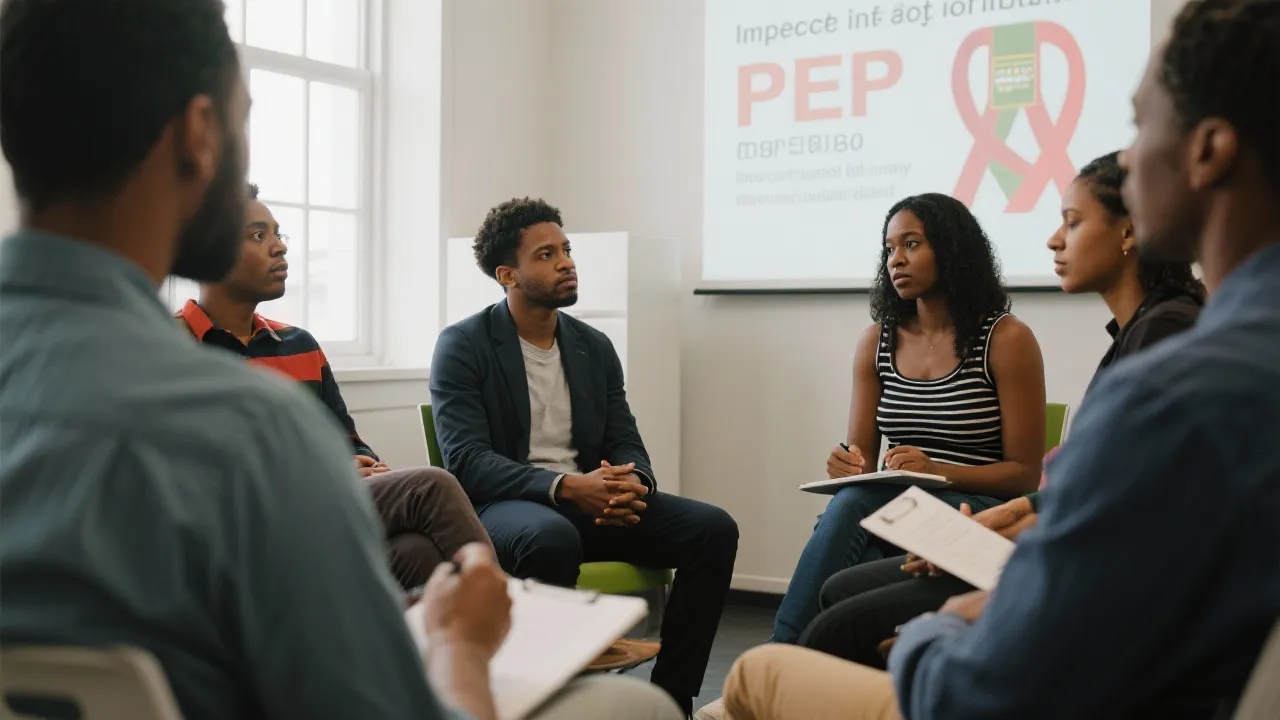
Public health initiatives are essential in navigating these challenges. Educational programs that highlight the importance of PrEP, coupled with community outreach, can significantly aid in increasing awareness and reducing stigma. Furthermore, advocating for policies that improve access to PrEP, including subsidized programs and insurance coverage, is vital in making this life-saving option available to those who need it most. Historically, initiatives that combine education, stigma reduction, and accessibility efforts have shown promise in increasing PrEP uptake in various regions.
The future of PrEP in HIV prevention looks promising, with ongoing research focused on developing long-acting formulations that require less frequent dosing. Innovations such as injectable PrEP, which may only need to be administered every few months, could overcome some of the barriers associated with daily oral regimens. As clinical trials progress, evidence of efficacy and safety profiles will shape the approval and rollout of such alternatives.
In addition to injectable formulations, research is also investigating long-acting implants and alternative delivery methods, including topical gels or microbicides. These innovations could revolutionize the ways in which individuals engage with preventive measures, creating more options tailored to personal preferences and lifestyles. For example, a self-administered gel could empower individuals to take charge of their prevention strategies in a discreet way.
Moreover, increasing public health initiatives focused on education and reducing stigma holds potential to expand access and uptake of PrEP, especially in vulnerable communities. Exploring partnerships with community organizations and influencers within these populations fosters trust and encourages conversations around sexual health. Leveraging social media for outreach and engagement can also attract younger demographics who may be at risk but lack information about available preventive measures.
| Formulation | Pros | Cons |
|---|---|---|
| Daily Oral PrEP | High effectiveness with consistent use | Requires daily adherence; accessibility issues |
| Injectable PrEP (Under Development) | Reduces frequency of dosing | Still undergoing trials; accessibility to be determined |
| Implantable PrEP (Under Research) | Long-term protection with minimal adherence concerns | Invasive procedure; not widely available yet |
Q1: Who should consider taking PrEP?
A: PrEP is recommended for individuals at high risk of HIV exposure, including those with HIV-positive partners, people who have multiple sexual partners, and individuals who inject drugs. Additionally, men who have sex with men and those who engage in unprotected sex or have a sexually transmitted infection (STI) are also prime candidates for this preventive measure.
Q2: Are there any side effects associated with PrEP?
A: Some users experience side effects such as nausea or headaches when starting PrEP, but these often subside. It's important to discuss any concerns with a healthcare provider. In rare cases, PrEP may cause kidney issues, thus regular monitoring at a healthcare facility is essential for those on long-term treatment. Proper medical supervision ensures interventions can be made should complications arise.
Q3: How can I access PrEP?
A: PrEP can be accessed through healthcare providers who will assess your risk and discuss the top options available for you. In some regions, there are also clinics and community organizations that provide support for accessing PrEP. It is increasingly available in pharmacies, and many health systems have adopted streamlined procedures for prescription renewals.
Q4: Is PrEP effective against all strains of HIV?
A: Yes, PrEP is effective against all known strains of HIV. It provides comprehensive protection by inhibiting the virus regardless of its subtype, which is particularly important in regions where multiple strains may circulate.
Q5: Can PrEP be used alongside other preventive measures?
A: Absolutely! PrEP can be used in combination with other prevention methods, such as condoms and regular testing for STIs. This layered approach maximizes protection and promotes overall sexual health.
The impact of PrEP on HIV prevention is profound and multifaceted. As a powerful tool in the fight against HIV, its potential to drive down transmissions is contingent upon addressing the barriers to its adoption and ensuring widespread access. With continued research and community engagement, PrEP can decisively alter the landscape of HIV prevention strategies, steering the world closer toward controlling an epidemic that has persisted for decades.
Moreover, as global health policy continues to evolve, integrating PrEP into broader health care systems is imperative. This integration not only amplifies the potential for lowering infection rates but also ensures that those at risk receive comprehensive healthcare, which may include mental health support, counseling, and education on sexual health. By adopting a holistic view of health that encompasses the social determinants of health—such as access to education, healthcare, and social support—the global community can create a conducive environment for the prevention of HIV and other sexually transmitted infections.
Ultimately, the success of PrEP, much like any public health intervention, relies heavily on collaboration among healthcare providers, researchers, policymakers, and communities. As we advance into a new era of HIV prevention, it is crucial to foster open dialogue, enhance education initiatives, and commit to policies that prioritize and protect the sexual health of all individuals. In doing so, we pave the path toward an HIV-free future, where stigma and fear are replaced with knowledge, empowerment, and effective prevention strategies.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
