This guide delves into the evolving landscape of Anti-HIV medicine, offering insight into its mechanisms, importance, and accessibility. Anti-HIV drugs are pivotal in controlling and managing HIV. They work by inhibiting the virus's ability to replicate, thus reducing the viral load in the bloodstream and preventing disease progression. These medications are critical not only for increasing the longevity and quality of life of those with HIV but also for reducing the risk of transmission.

In the past few decades, the development of Anti-HIV medicines has significantly transformed the prognosis for individuals diagnosed with the Human Immunodeficiency Virus (HIV). These medications, commonly referred to as antiretrovirals (ARVs), work by targeting various stages of the virus's life cycle, thereby preventing it from replicating and progressing to Acquired Immunodeficiency Syndrome (AIDS). As we dive into the specifics of these life-saving drugs, we will explore their types, mechanisms, and the crucial role they play in contemporary health care. This understanding not only helps in appreciating the medication's efficacy but also in acknowledging the social, financial, and personal contexts surrounding its use.
The landscape of Anti-HIV medicine includes various classes of drugs, each targeting different phases of the HIV replication process:
Understanding how these medications work on a molecular level is crucial for realizing their importance in managing HIV. Each class of drugs operates through unique mechanisms:
Anti-HIV medicine has revolutionized the treatment paradigm for HIV-infected individuals. When taken as prescribed, these medications can effectively reduce the viral load to undetectable levels, which vastly improves the patient's quality of life and longevity. Moreover, maintaining an undetectable viral load significantly lowers the risk of HIV transmission, forming the basis of the 'Undetectable = Untransmittable' (U=U) campaign. This underscores the dual benefit of treatment: personal health and public safety.
Beyond the clinical implications, the availability of ARVs has also initiated crucial sociopolitical discussions about healthcare equity and human rights. The juxtaposition of a potentially life-threatening virus with the ability to manage it through medication has prompted calls for universal healthcare coverage and the abolishment of stigma against people living with HIV.
Recent years have witnessed notable advancements in Anti-HIV therapy. These include the development of single-tablet regimens that simplify treatment adherence by combining multiple drugs into one pill, significantly improving adherence rates. This is especially crucial in populations that face barriers to medication adherence, such as those with busy lifestyles or mental health issues. For instance, the Atripla regimen combines Efavirenz, Emtricitabine, and Tenofovir, allowing patients to take one pill once daily instead of managing multiple prescriptions.
Furthermore, long-acting injectables are emerging as an alternative for individuals who struggle with daily pill intake, offering monthly or even bimonthly dosing. These innovative forms of medication can reduce care gaps and minimize the chances of treatment failure associated with missed doses. Recent studies suggest that long-acting cabotegravir and rilpivirine are as effective as traditional daily oral therapies. This option enlarges the treatment landscape, providing choices that cater to individual patient preferences.
Another promising area of research is the investigation of therapeutic vaccines that could enhance immune responses to HIV. While preventive vaccines are critical, therapeutic vaccines could help those already infected manage their condition better, potentially leading to an HIV-free future.
Ensuring access to Anti-HIV medicine is a global health priority. Various international initiatives aim to provide these drugs at low or no cost to regions hardest hit by the epidemic. The Global Fund, PEPFAR, and local health organizations are instrumental in broadening access to these crucial medications, emphasizing the importance of equitable healthcare in controlling the epidemic.
Additonally, numerous generic versions of antiretrovirals facilitate greater affordability. The use of generics has significantly reduced the cost of treatment in developing countries, where healthcare budgets are constrained. Countries like India have become well-known for their production of generic antiretrovirals, which are essential in global health efforts to combat HIV.
However, challenges remain regarding access to the latest and most effective formulations, particularly in low-income regions. Policy reforms promoting intellectual property laws that enable wider distribution of generics, as well as increased funding for HIV care, are essential to ensure that treatment is available to all who need it.
| Organization | Role in Anti-HIV Efforts |
|---|---|
| The Global Fund | Provides funding for comprehensive HIV care and treatment initiatives worldwide, helping countries to scale up their responses to the epidemic. |
| PEPFAR (President’s Emergency Plan for AIDS Relief) | Directs resources towards ARV procurement and distribution, particularly in high-prevalence regions, and supports healthcare infrastructure development. |
| Local NGOs | Act as facilitators in delivering Anti-HIV medicine and ensuring adherence to treatment protocols, often engaging with communities to provide education and support. |
| WHO (World Health Organization) | Establishes guidelines for HIV treatment and prevention, ensuring comprehensive care standards are met across different regions. |
While significant progress has been made, challenges remain, such as drug resistance, adverse effects, and maintaining lifelong adherence to therapy. Drug resistance can occur when the virus mutates and does not respond to certain medications, which can limit treatment options and complicate management. Regular monitoring of the viral load and resistance testing allows clinicians to adjust treatment plans proactively and maintain efficacy.
Adverse effects present another layer of complexity in treatment. While many individuals tolerate ARVs well, some experience debilitating side effects that may lead to discontinuation of therapy. Side effects can vary depending on the class of medication prescribed. For instance, NNRTIs are often associated with central nervous system effects, while PIs might cause gastrointestinal issues. Continuous communication between healthcare providers and patients is crucial for managing these effects and ensuring adherence to treatment schedules.
Maintaining lifelong adherence to therapy is paramount; missed doses can lead to uncontrolled viral replication and subsequently to resistance. The stigma associated with being HIV positive can also hinder adherence, as individuals may fear judgment or discrimination. Culturally sensitive education and support initiatives are necessary to address these barriers.
Social support systems such as peer groups and family involvement help foster adherence. Mental health screenings and treatment for issues like depression can enhance the likelihood of adherence, emphasizing the need for a holistic approach to care.
Developing novel strategies to enhance medication adherence is vital in ensuring effective management of HIV. Technology can play a crucial role in this regard:
The strides made in Anti-HIV medicine underscore monumental achievements in public health, marking a transition from an invariably fatal diagnosis to a manageable chronic condition. Continued investment in research, access, and education is imperative to sustaining these gains and approaching the ultimate goal of ending the HIV epidemic. As we continue to adapt and innovate, Anti-HIV medicine serves as a beacon of hope and resilience in the realm of medical science.
Looking Forward: Innovations on the Horizon
The future of Anti-HIV therapies is bright as research continues to unravel new avenues for treatment. Scientists are exploring gene editing technologies, which could offer insights into potential cures. Studies involving CRISPR technology aim to remove HIV DNA from infected cells, highlighting the potential for a complete eradication of the virus from an individual's body.
Furthermore, the focus on preventive measures through vaccine development remains a critical area. In addition to therapeutic vaccines that enhance immunity in those already infected, researchers are also investigating preventive vaccines that could stop HIV transmission altogether. The ongoing studies highlight a collective vision to eradicate the epidemic by combining effective treatment with prevention strategies.
As more options emerge, comprehensive care models that address both the medical and psychosocial needs of individuals affected by HIV will be essential. A multidimensional approach ensures that the progress made is not only maintained but also expanded upon, ultimately fostering a healthier society where individuals with HIV can thrive without stigma.
Explore the Tranquil Bliss of Idyllic Rural Retreats

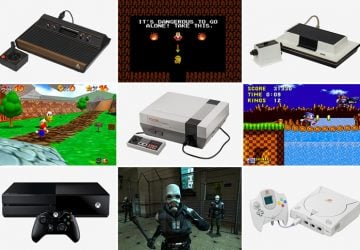
Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!
Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
