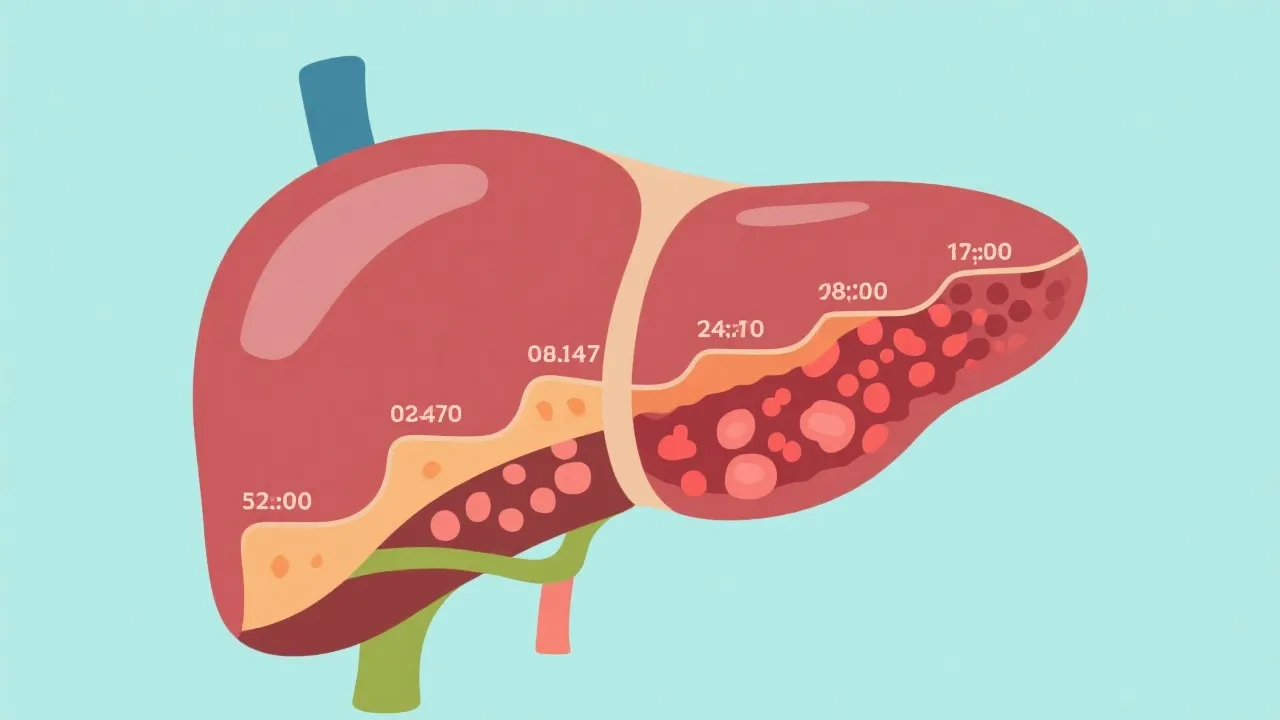
Non-alcoholic fatty liver disease (NAFLD) and hepatocellular carcinoma (HCC) are significant liver health concerns. NAFLD is characterized by excessive fat storage in liver cells, potentially leading to inflammation and scarring. If unchecked, it may progress to HCC, a primary type of liver cancer. Understanding their relationship is vital for healthcare strategies and patient outcomes.
Non-alcoholic fatty liver disease (NAFLD) is increasingly prevalent worldwide, affecting millions due to its association with obesity, metabolic syndrome, and sedentary lifestyles. NAFLD encompasses a spectrum of liver conditions, from simple steatosis to the more severe non-alcoholic steatohepatitis (NASH), which can progress to cirrhosis and hepatocellular carcinoma (HCC). Understanding this progression is critical for developing effective prevention and treatment strategies. As the prevalence of NAFLD continues to rise globally, the connection between NAFLD and HCC becomes a pressing public health concern that calls for immediate action and attention.
The rise of NAFLD correlates with global increases in obesity and diabetes. According to recent global health reports, approximately 25% of the adult population is affected by NAFLD, with this number projected to increase dramatically in the coming decades. In simple terms, NAFLD is the accumulation of excess fatty acids in liver cells, not attributed to alcohol consumption. The condition is often asymptomatic in its early stages, making early detection challenging. However, clinical studies have shown that while many individuals may not experience symptoms, the disease poses significant risks if it evolves into NASH, characterized by liver inflammation and damage. This inflammation triggers a cascade of cellular events leading to fibrosis, which is the scarring of liver tissue. NASH can lead to fibrosis, cirrhosis, and eventually HCC, a primary liver cancer that accounts for a substantial portion of cancer-related mortality globally. In fact, HCC is considered one of the fastest-growing causes of cancer-related deaths worldwide, underscoring the importance of addressing NAFLD as a key contributor to this alarming trend.
The transition from NAFLD to HCC is complex and involves multiple biochemical and molecular changes within the liver environment. Chronic inflammation in NASH promotes a fibrogenic response, where ongoing liver injury results in scarring. Over time, cirrhosis can develop, creating a setting ripe for malignant transformations. This pathway involves a series of pathological processes, including lipid peroxidation, mitochondrial dysfunction, and the induction of genomic instability, all of which contribute to hepatocyte damage. Key factors contributing to this risk include genetic predispositions, lifestyle, and environmental influences. For instance, individuals with certain genetic polymorphisms related to lipid metabolism may be at higher risk for progressing from simple steatosis to NASH, subsequently leading to cirrhosis and HCC. Furthermore, environmental factors such as exposure to toxins and the presence of comorbid conditions like diabetes and hypertension exacerbate these risks. Understanding these interconnected pathways can aid in developing targeted therapies and interventions aimed at halting disease progression before it reaches the carcinogenic stage.
Preventing the progression of NAFLD to HCC necessitates a multi-faceted approach. Lifestyle modifications, such as maintaining a healthy weight through diet and physical activity, are foundational. The implementation of structured lifestyle intervention programs specifically tailored to individuals at risk for NAFLD has shown promise in reducing liver fat and improving overall metabolic health. Regular screening and monitoring are also crucial, especially for those at heightened risk due to metabolic disorders or family history. Medical professionals stress the importance of liver function tests and imaging to monitor disease status and the effectiveness of interventions. These monitoring strategies may include periodic ultrasounds, elastography for measuring liver stiffness (a surrogate marker for fibrosis), and assessments of serum biomarkers, which can provide meaningful insights into liver health. It’s essential to cultivate a proactive health culture where patients are informed about the risks and benefits of monitoring their liver health, thus enabling early intervention when necessary.
While lifestyle changes remain the cornerstone of managing NAFLD, medical treatments are advancing rapidly. Several pharmacological agents targeting metabolic pathways are under investigation, with some showing promise in halting or reversing disease progression. For instance, drugs like pioglitazone and vitamin E have been shown to improve histological features in patients with NASH. Additionally, the investigation of novel classes of medications aimed at reducing liver inflammation and fibrosis is ongoing, providing hope for more effective treatment strategies in the future. For individuals diagnosed with liver cirrhosis or HCC, treatment options range from surgical resection and liver transplantation to newer techniques like transarterial chemoembolization (TACE) and radiofrequency ablation (RFA). The choice of treatment can be complex and hinges on several factors, including tumor size, liver function, and the presence of underlying liver disease. Moreover, advancements in immunotherapy are beginning to show promise, offering potential new avenues for treatment that leverage the body’s immune system to fight cancer.
| Aspect | NAFLD Management | HCC Management |
|---|---|---|
| Focus | Lifestyle changes, metabolic control | Tumor reduction, liver preservation |
| Treatment Modalities | Diet, exercise, glucose-lowering drugs | Surgery, targeted therapy, immunotherapy |
| Monitoring | Regular blood tests, liver imaging | Frequent MRI, AFP level monitoring |
Experts in the field advocate for an integrated approach that combines personalized medicine with broader public health initiatives. Genetic research is unlocking potential predictive markers that could revolutionize early intervention strategies. Biomarkers that reflect the degree of liver inflammation and fibrosis are being explored as tools to stratify patients at risk of progressing to HCC. Additionally, public awareness campaigns can educate communities on the importance of liver health and the implications of NAFLD as a significant precursor to HCC. The establishment of multidisciplinary teams that include hepatologists, nutritionists, and exercise physiologists is increasingly recognized as essential for providing comprehensive care. These teams can work collaboratively to create individualized management plans that can improve patient outcomes and quality of life.
For healthcare professionals and patients alike, understanding the link between NAFLD and HCC is crucial. Increased education surrounding lifestyle modifications, early screenings, and management strategies for both NAFLD and HCC can lead to better outcomes. By harnessing the latest research and technological innovations, there is hope for improved outcomes and potential breakthroughs in liver disease management. While the road from discovery to treatment is long, the continued dedication from researchers and clinicians holds promise for those affected by these challenging conditions. The integration of care, research, and community awareness will be paramount in combating the increasing prevalence of NAFLD and its progression to HCC.
NAFLD and HCC not only have profound implications for individual health but also pose significant challenges to healthcare systems worldwide. The economic burden of these diseases is substantial, affecting billions in healthcare costs and loss of productivity. As NAFLD progresses to more severe stages, the need for healthcare resources escalates, resulting in increased demands on hospitals and specialized care facilities. Public health initiatives aimed at reducing obesity and diabetes prevalence are crucial to mitigating the rise of NAFLD and its consequent evolution into HCC. Educating the community about the risks of fatty liver disease and the essential lifestyle changes could potentially lead to a decrease in new cases and improve overall public health.
The global rise of NAFLD and HCC is not confined to any particular demographic or geographic region. Countries worldwide must recognize the patterns of increasing incidence and rising health complications associated with these diseases. For example, while NAFLD was historically linked to western diets high in sugar and unhealthy fats, it is increasingly being diagnosed in regions with different dietary habits, such as Asia and Middle Eastern countries, showcasing how lifestyle factors can transcend cultural boundaries. International collaborations are essential to share research findings, treatment protocols, and effective public health strategies. Countries facing different prevalence levels can learn from each other regarding successful interventions and care models, ensuring a more coordinated global response to these liver diseases.
The ongoing research into NAFLD and HCC is critical in advancing our understanding and management of these diseases. Scientific exploration is focusing on a wide array of factors ranging from metabolic pathways to gut microbiota's influence on liver health. Clinicians and researchers are increasingly emphasizing the need for multidisciplinary studies that explore not only the biochemical aspects of NAFLD but also the behavioral and societal factors contributing to its rise. Large-scale epidemiological studies are necessary to evaluate the effectiveness of new interventions and treatments while considering the diverse populations affected by these diseases. Encouraging collaboration between academia, industry, and healthcare providers can accelerate the development of novel therapies and diagnostic tools.
Patients with NAFLD or HCC can take an active role in their health by adopting self-management strategies. Understanding the disease process, recognizing risk factors for progression, and maintaining regular communication with healthcare providers are central to effective disease management. Empowering patients with education and resources allows them to make informed decisions about their health. Support groups can also play a crucial role in providing emotional support and sharing strategies for lifestyle changes, thus promoting adherence to healthier choices. The integration of technology, such as mobile health applications that aid in tracking dietary habits and physical activity, can further enhance patient engagement and self-management efforts.
Understanding the connection between NAFLD and HCC is fundamental in addressing the rising burden of liver diseases worldwide. Strategies encompassing prevention, early detection, and comprehensive management hold the key to mitigating the impacts of these conditions. A focus on patient education, community awareness, and a multidisciplinary approach in research and treatment can yield significant advancements in the fight against NAFLD and its potential progression to HCC. As we learn more about these complicated relationships between lifestyle, metabolic health, and liver disease, ongoing commitment from the medical community will help in combating these formidable diseases, ultimately leading to better health outcomes for all.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
