Nonalcoholic Steatohepatitis (NASH) is a progressive liver disease marked by inflammation and damage caused by fat accumulation in the liver. Unlike alcohol-induced liver conditions, NASH develops independently of alcohol consumption, often associated with metabolic syndromes such as obesity and diabetes. The increasing prevalence highlights the need for effective awareness and management strategies.
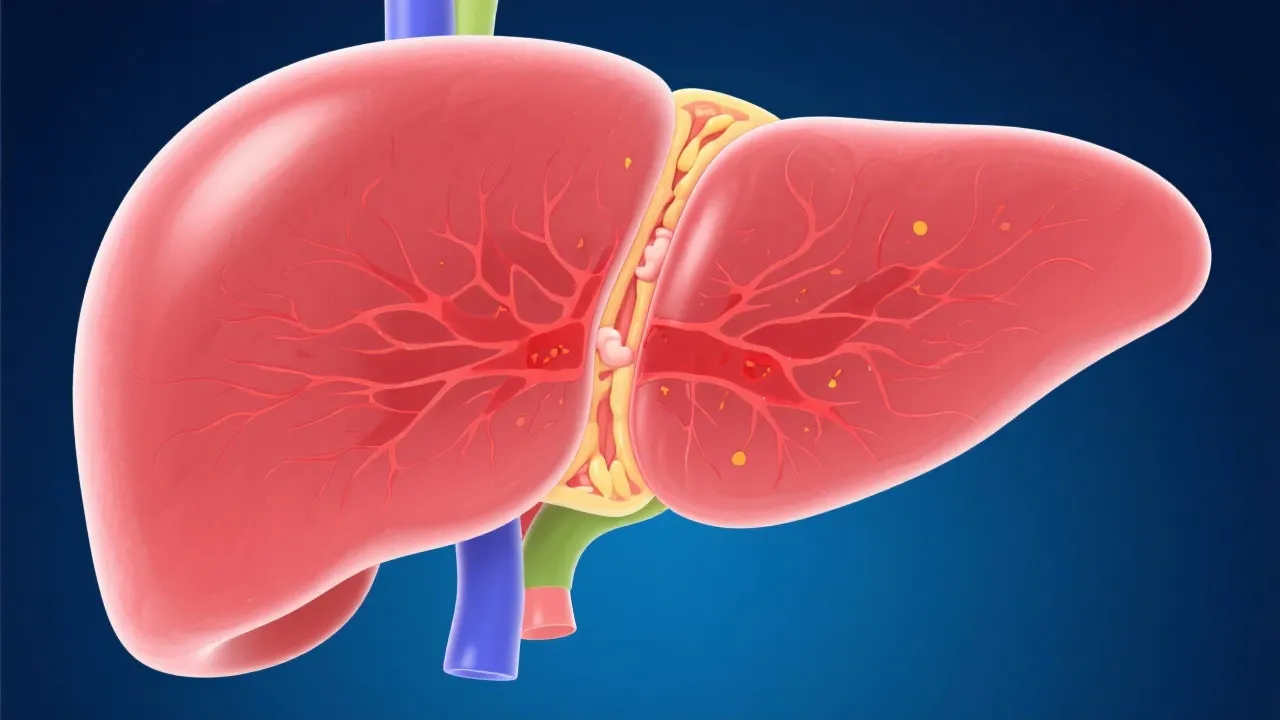
Nonalcoholic Steatohepatitis (NASH) has emerged as a significant public health concern due to its progressive nature and the potential to lead to more severe liver conditions, such as cirrhosis and liver cancer. It is important to note that NASH is associated with a spectrum of liver diseases, collectively termed nonalcoholic fatty liver disease (NAFLD). Within this spectrum, NASH is characterized by liver inflammation and damage due to excess fat accumulation, occurring independently of significant alcohol consumption. This dual nature—steatosis combined with inflammation—distinguishes NASH from other liver conditions, emphasizing the complexity of its pathology. Moreover, the clinical implications of NASH extend beyond hepatic complications, influencing other systemic conditions such as cardiovascular disease and metabolic syndrome. Understanding these relationships is critical for effective management and prevention of the condition.
The characterization of NASH as an expanding clinical entity reflects its growing recognition as a condition of considerable medical and social importance. The increasing incidence correlates with the global rise in obesity, diabetes, and related metabolic disorders, with statistical evidence showing alarming trends particularly in developed nations. Current statistics suggest that NASH affects approximately 3-5% of the adult population, with higher rates in populations with prevalent metabolic syndrome, which includes hypertension, dyslipidemia, and insulin resistance. This underscores the importance of early detection and lifestyle interventions to curb disease progression. Furthermore, demographic studies show that certain ethnic populations, particularly Hispanic and Asian communities, experience higher rates of NASH, which raises important considerations regarding screening practices and tailored prevention strategies.
NASH develops as a result of fat accumulation in liver cells, leading to cell damage, inflammation, and, potentially, fibrosis. The liver, being a central metabolic organ, plays a pivotal role in lipid metabolism, and its dysregulation can prompt steatosis. This condition is often asymptomatic in its early stages, complicating timely diagnosis. The pathophysiology involves complex interactions between genetic predispositions, diet, and environmental factors, which together result in insulin resistance and oxidative stress. Genetic factors include polymorphisms in genes associated with lipid metabolism, such as the PNPLA3 gene, which has been identified as a major risk factor for NASH. These elements underscore the importance of understanding individual patient profiles for effective management strategies. Emerging studies are also focusing on gut microbiota's role in modulating liver inflammation and fat accumulation, suggesting a potential target for therapeutic interventions.
Diagnosing NASH necessitates a comprehensive approach due to its silent progression. Evaluations often involve liver function tests (LFTs), imaging modalities like ultrasound and MRI, and, in some cases, liver biopsy for exact staging. Liver function tests help assess the extent of liver dysfunction, although they can be normal even in significant liver disease. Non-invasive imaging, such as elastography, has gained attention for its ability to evaluate liver stiffness, which correlates with fibrosis. Innovations in non-invasive diagnostic tools are promising for assessing liver fibrosis degree without invasive procedures, enhancing patient comfort and compliance. These advancements, including serum biomarker panels and proprietary algorithms, are critical for early-stage identification, which is crucial in preventing the disease's progression to cirrhosis. As research evolves, the hope is to find a reliable test that can effectively differentiate between simple steatosis and NASH, particularly in individuals with risk factors but no overt symptoms.
| Diagnostic Tool | Method | Advantage | Limitation |
|---|---|---|---|
| Ultrasound | Imaging technique for liver fat estimation | Non-invasive, widely available | Less sensitive in detecting inflammation and fibrosis |
| MRI | Detailed imaging for fat and fibrosis | High sensitivity and specificity | Costly and less accessible in certain regions |
| Liver Biopsy | Histological examination | Definitive diagnosis | Invasive, risk of complications and sampling error |
| Elastography | Non-invasive measurement of liver stiffness | Indicates fibrosis with a good correlation | Operator-dependent, less effective in obesity |
| Serum Biomarkers | Blood tests evaluating specific liver enzymes and factors | High potential for non-invasive assessment | Still under research, not widely validated for clinical use |
Currently, there is no FDA-approved medication specifically for NASH, making lifestyle modification the frontline approach. Weight loss through diet and exercise has shown to improve liver pathology significantly, with studies indicating that a weight reduction of 7-10% can lead to histological improvements. Additionally, dietary modifications emphasizing a Mediterranean diet, which is rich in healthy fats, whole grains, fruits, and vegetables, are being recommended due to their beneficial effects on insulin sensitivity and liver health. Emerging therapies targeting metabolic pathways and fibrosis are under clinical trials, offering hope for future pharmacological interventions. These include agents aimed at reducing liver fat, mitigating inflammation, and preventing fibrosis progression. Investigational drugs such as FXR agonists and ACC inhibitors are showing promise, with ongoing studies assessing their efficacy and safety. Engaging patients in a thorough understanding of their condition and treatment options is vital for adherence and success in disease management. Behavioral counseling to support lifestyle changes is equally important, as psychosocial aspects can significantly influence an individual’s ability to make lasting health improvements.
The scientific community is actively exploring new therapeutic targets within the pathways of lipid metabolism, inflammation, and fibrogenesis. Encouraging results from recent trials of agents such as obeticholic acid and saroglitazar demonstrate potential in slowing disease progression. Obeticholic acid, a farnesoid X receptor (FXR) agonist, has shown promising results in improving liver histology in patients with NASH and is undergoing additional studies to confirm its long-term efficacy. Similarly, saroglitazar, a dual PPAR alpha and PPAR gamma agonist, has demonstrated improvements in liver stiffness and metabolic profiles in clinical trials. These innovations signal a paradigm shift in treatment protocols, emphasizing personalized medicine based on patient-specific genetic and environmental factors. Furthermore, the exploration of combination therapy approaches is gaining interest, where patients may benefit from multiple therapeutic strategies to manage both the metabolic and hepatic aspects of NASH, underscoring the complexity of the disease and the need for multifactorial interventions.
Healthcare providers play a crucial role in managing NASH through education, regular monitoring, and the encouragement of lifestyle interventions. A comprehensive understanding of the disease among healthcare professionals is essential, as it enables the identification of at-risk populations and the appropriate implementation of screening measures. Coordination between hepatologists, endocrinologists, nutrition experts, and primary care physicians is vital for a multidisciplinary approach, ensuring comprehensive patient care. Moreover, continuous medical education and awareness campaigns can enhance the understanding of NASH not just among healthcare providers, but also among the general public. This is particularly important for understanding the risk factors associated with the disease, including metabolic components and lifestyle choices. Collaborating with community health organizations to promote awareness of NASH, alongside regular check-ups for at-risk patients, can greatly improve early detection and intervention efforts.
Nonalcoholic Steatohepatitis represents a growing clinical challenge as its impact on public health becomes increasingly evident. The complexity of its pathophysiology, coupled with the rising prevalence of associated risk factors, necessitates a comprehensive and proactive approach to management. Addressing this complex condition requires a multifaceted strategy encompassing early diagnosis, lifestyle management, and emerging pharmacologic therapies. Increasing awareness about the condition, enhancing patient education, and optimizing care can significantly mitigate the burden of NASH and improve patient outcomes. Furthermore, as research continues to evolve, there is an optimistic outlook for future treatment possibilities that can potentially transform the care landscape for individuals with NASH. By fostering a collaborative effort involving healthcare providers, patients, and the broader community, we can hope to better control and reverse the trajectory of this disease, ultimately leading to improved health outcomes and quality of life for affected individuals.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
