Liver transplantation has evolved as a critical treatment for Non-Alcoholic Steatohepatitis (NASH), a severe form of non-alcoholic fatty liver disease. Growing prevalence of NASH necessitates a closer examination of transplantation as viable intervention amidst limited alternatives.
In the realm of medical progress, liver transplantation has emerged as a pivotal option for patients grappling with the severe implications of Non-Alcoholic Steatohepatitis (NASH). As an advanced stage of non-alcoholic fatty liver disease (NAFLD), NASH leads to inflammation and damage akin to that caused by heavy alcohol use, despite the absence of alcohol consumption. With a rising number of individuals affected, understanding the pathway from NASH to liver transplantation becomes crucial. The implications of NASH are multifaceted, impacting not only the physical well-being of patients but also their psychological health, social dynamics, and economic status.
Non-Alcoholic Steatohepatitis, better known as NASH, is garnering attention as a significant public health challenge worldwide. The transition from fatty liver to cirrhosis or liver cancer makes the situation alarming. Experts pinpoint its prevalence due to lifestyle factors such as poor diet and sedentary behavior, alongside metabolic syndromes including obesity and diabetes. A staggering rise in obesity rates over recent decades has been identified as a prime contributor to NASH, particularly in developed countries. The World Health Organization (WHO) reports that obesity has nearly tripled since 1975, and coupled with dietary habits high in sugar and fat, this situation is exacerbating the prevalence of NASH.
Additionally, NASH is not just a localized epidemic; it has global consequences. The economic burden associated with NASH includes healthcare costs for treating liver-related conditions, lost productivity due to illness, and costs incurred from liver transplantation procedures. As a significant contributor to liver disease mortality, NASH calls for urgent attention and strategic interventions at multiple levels — prevention, early detection, and management.
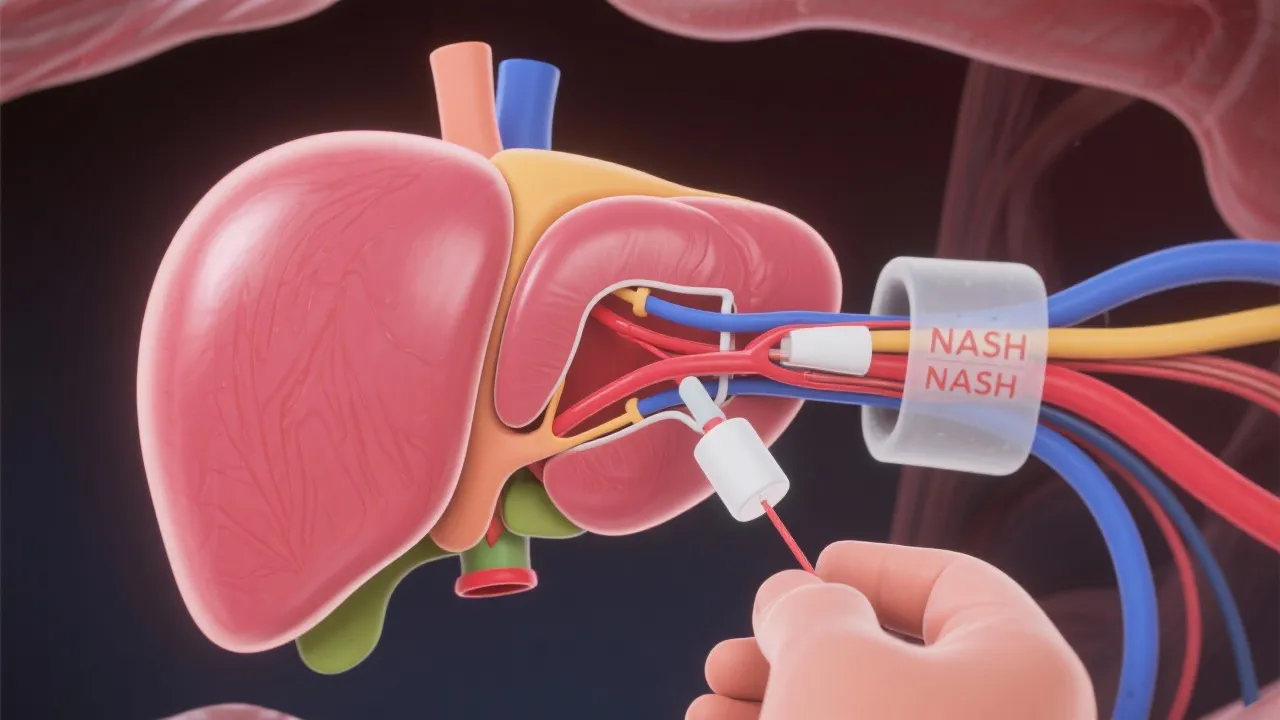
Liver transplantation involves replacing a diseased liver with a healthy one from a donor. It is recommended when liver damage reaches a point where it cannot function adequately to sustain life. For NASH patients, liver transplantation becomes a necessary recourse when the disease progresses to liver failure or cirrhosis. The goal is to restore the liver's function, potentially extending and improving the quality of life. The transplantation process can be daunting, and many patients often experience a mix of hope and anxiety prior to the procedure. Understanding the fundamentals can help demystify the process and prepare patients and their families for the journey ahead.
Moreover, there are two primary types of liver transplantation: orthotopic and living donor transplantation. Orthotopic transplantation involves the complete removal of the diseased liver and replacement with a donor liver, whereas living donor transplantation allows for a portion of a healthy person's liver to be transplanted. The living liver has the remarkable ability to regenerate, making this a viable and often life-saving option for patients.
NASH-induced liver failure occurs when liver cells are substituted by scar tissue (fibrosis), leading to cirrhosis. The irreversibility of cirrhosis necessitates liver transplantation, especially when complications such as ascites, hepatic encephalopathy, or variceal bleeding arise. The transition from simple steatosis to NASH and ultimately cirrhosis is often insidious, often going unnoticed until significant damage has occurred. Current pharmacological treatments for NASH are notably limited and primarily focus on managing associated conditions like diabetes and obesity. Because the disease progression can be so slow, many individuals remain unaware of their increased risk until they face severe health consequences.
Furthermore, certain genetic predispositions can exacerbate the risks of developing NASH and cirrhosis. Research is underway to identify genetic markers and develop treatments tailored to those at higher risk. Understanding the pathophysiology of NASH helps healthcare providers implement effective risk management strategies, ultimately aiming to circumvent the dire need for transplantation.
Outcomes post-liver transplantation for NASH generally parallel those of transplants for other causes. Several studies highlight five-year survival rates exceeding 75%, a testament to the procedure's efficacy despite the challenges posed by underlying metabolic conditions. Continuous follow-up and management of contributing factors such as obesity are imperative post-transplant. The success of the transplant is not solely determined by the surgery but also significantly influenced by the patient's commitment to lifestyle changes and follow-up care.
Moreover, studies have suggested that patients with NASH who undergo liver transplantation may have a different prognosis compared to those with alcoholic liver disease or viral hepatitis. Ongoing research into long-term outcomes and the effectiveness of interventions post-surgery is vital for improving the quality of care provided to individuals with NASH. Comprehensive care models that include nutritional counseling, exercise programs, and psychological support contribute to higher success rates and improved patient satisfaction.
Although liver transplantation presents a beacon of hope for patients with NASH, it isn't without challenges. The scarcity of available livers juxtaposed with rising demand highlights ethical and logistical conundrums in allocation. Each year, thousands of patients await liver transplantation, with many facing long waits and potential deterioration of their health conditions during this period. This raises critical questions about prioritization based on medical urgency and the overall benefit to the healthcare system.
Aside from availability, socioeconomic disparities and access to healthcare resources often dictate who receives priority, emphasizing the need for equitable healthcare practices. Socioeconomic status has been shown to influence not only access to transplant centers but also factors such as adherence to post-operative care, nutritional support, and lifestyle modifications essential for positive outcomes. Efforts are underway to create outreach programs aimed at educating underserved populations about liver health and the options available for individuals with NASH.
Furthermore, addressing the stigma associated with liver disease—often linked with lifestyle choices—remains an essential aspect of broadening understanding and support for NASH patients. This stigma can affect mental health outcomes and willingness to seek treatment or accept the need for lifestyle transformations.
Promoting lifestyle changes forms a cornerstone of preventing and managing NASH. Emphasizing balanced nutrition and physical activity can mitigate progression and improve overall health. This is crucial, particularly prior to consideration for transplantation, as healthier individuals fare better post-surgery. Weight loss, when appropriate, has been cited as one of the most significant factors in slowing disease progression.
Moreover, patient education regarding dietary changes is important. A diet rich in fruits, vegetables, whole grains, and lean proteins can reduce the liver's fat content and improve insulin sensitivity. Incorporating regular physical activity, tailored to individual capabilities, can enhance liver health and overall wellbeing. Many healthcare providers now advocate for a multidisciplinary approach that includes dieticians and exercise physiologists as part of the care team for patients at risk of or currently managing NASH.
This behavioral modification does not only apply to pre-transplant patients but should be a continuous goal post-transplant. Long-term lifestyle adjustments support the health of the newly transplanted liver and decrease the risk of developing further liver complications.
As the incidence of NASH continues to climb, liver transplantation remains an essential yet complex facet in managing this debilitating condition. Innovative approaches are emerging, including pharmacotherapy targeting the underlying mechanisms of NASH. Agents that have shown promise in clinical trials include obeticholic acid and liraglutide, which aim not only to reduce liver fat but also to mitigate inflammation and fibrosis. These advancements signify potential shifts in treating the disease without necessitating transplantation in every case.
Ongoing research efforts are aimed at better understanding NASH pathogenesis and exploring potential pharmaceutical therapies. Collaborative efforts among researchers, clinicians, and organizations are focused on developing robust screening protocols, tailoring treatment plans, and raising awareness about the risks associated with NASH. These initiatives hold promise in reducing the dependency on transplantation, potentially alleviating the burden on both patients and healthcare systems. Increased advocacy for research funding into NASH will be paramount in driving improvements in patient outcomes and developing innovative therapeutic strategies.
| Factors | Considerations for NASH Transplant |
|---|---|
| Severity of Liver Damage | Cirrhosis and functional impairment necessitate transplantation. Regular monitoring of liver function tests and imaging studies can help gauge progress. |
| Availability of Donors | Limited by organ matching and donor availability. The implementation of programs that promote living donation can bridge this gap. |
| Post-Surgery Management | Includes risk mitigation through immunosuppressants and lifestyle adherence. Regular follow-ups facilitate early detection of complications. |
| Mental Health Support | Addressing the psychological aspect pre-and post-transplant is crucial for overall success. Providing resources for mental health support can improve compliance with treatment regimens. |
| Societal & Economic Factors | Income disparities can affect treatment access. Education and outreach programs are necessary to ensure equitable access to healthcare resources. |
The journey towards understanding and effectively managing NASH is multifaceted and is essential given the growing epidemic of liver disease worldwide. As liver transplantation remains one of the key interventions for patients with advanced NASH, an integrated approach combining medical, lifestyle, socioeconomic, and psychological perspectives will be imperative for improving health outcomes. Continuous research, patient education, and advocacy for equitable access to care can help alleviate the burden posed by NASH on individuals and healthcare systems alike. The path ahead is laden with challenges, but also immense potential for advancements in understanding and treating this complex disease.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
