Liver transplantation has emerged as a pivotal treatment for those afflicted by NASH, an advanced form of non-alcoholic fatty liver disease. The condition progresses from the accumulation of fat in liver cells to inflammation and scarring, ultimately requiring a transplant. This guide delves into the intricacies of liver transplantation for NASH, detailing its necessity, procedure, and common inquiries.
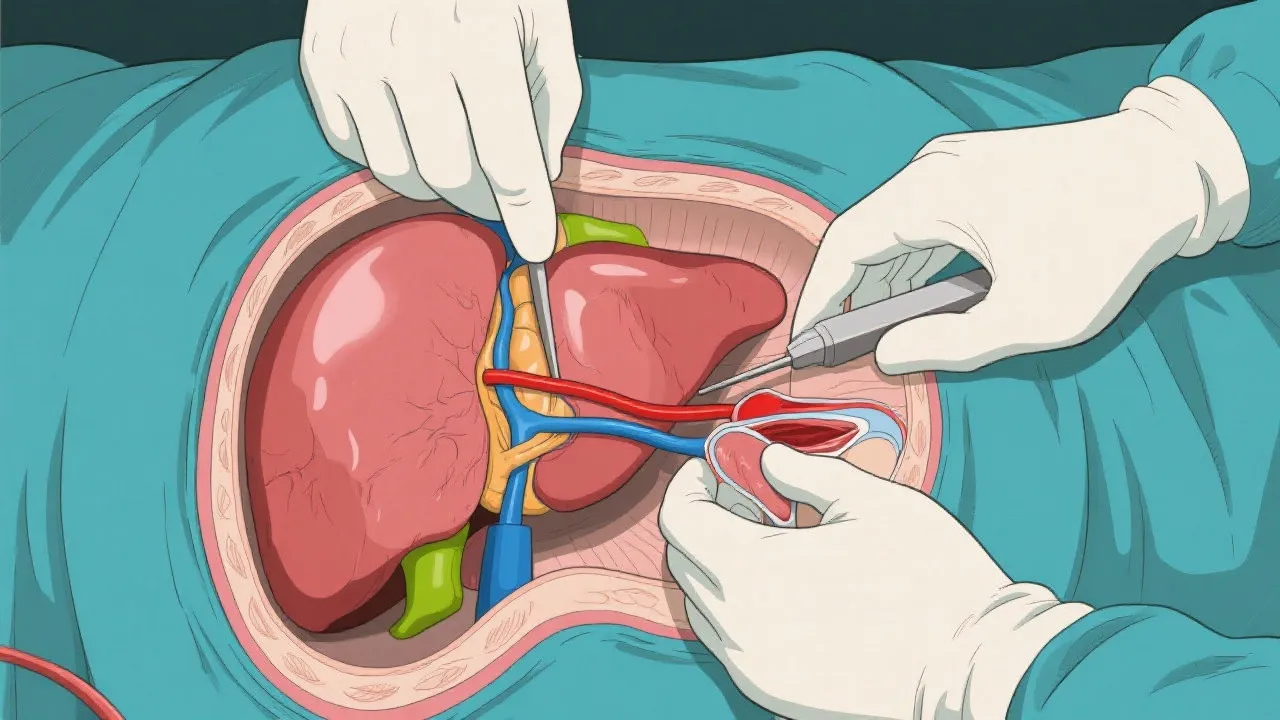
The prevalence of liver diseases necessitates a comprehensive understanding of available treatments, with liver transplantation standing out as a crucial intervention for certain advanced cases. Non-alcoholic steatohepatitis (NASH), a severe form of non-alcoholic fatty liver disease (NAFLD), can lead to progressive liver damage, making transplantation essential for patient survival. This article explores the relationship between NASH and liver transplants, offering a detailed perspective on the procedure's significance and implications. As the instances of obesity and related health issues rise globally, the correlation between these factors and liver disease underscores the urgent need to address both preventive strategies and treatment options.
NAFLD is characterized by excessive fat accumulation in the liver, often associated with obesity, diabetes, and metabolic syndrome. When simple fatty liver inflammation progresses, it can develop into NASH. This stage involves not only fat buildup but also liver cell inflammation and varying degrees of scarring (fibrosis). Over time, this can lead to cirrhosis, liver failure, or liver cancer, thus necessitating the possibility of a liver transplant.
Understanding NASH involves recognizing its risk factors and potential progression. Factors such as high cholesterol, hypertension, and sedentary lifestyle exacerbates the condition. Early stages of NAFLD may go unnoticed, as they often present with no symptoms. However, as liver damage escalates, patients may experience fatigue, discomfort in the upper right abdomen, and unexplained weight loss. If untreated, this can severely impact overall health and quality of life. Increased education and awareness about these symptoms can lead to earlier diagnosis and management, potentially delaying or even reversing the progression to NASH.
Liver transplantation is considered when NASH has advanced to the point of complete liver failure or in cases where there are no other viable treatment options. For many patients, a transplant becomes their lifeline, potentially returning them to a better quality of life after battling severe symptoms such as jaundice, fluid retention, and cognitive impairments.
Criteria for transplantation eligibility can vary but generally include the patient's overall health, the severity of liver disease as defined by specific scoring systems (such as the Model for End-Stage Liver Disease, or MELD score), and the absence of contraindications that could complicate the procedure, such as ongoing substance abuse or severe comorbidities. In some cases, patients may be placed on a waiting list for a suitable donor organ, and the urgency of transplantation can depend on how quickly their liver function is deteriorating. The transplant waiting period itself can often be fraught with anxiety and uncertainty, further underscoring the necessity for comprehensive pre-transplant counseling and support systems.
Recovery from liver transplantation can be lengthy, often requiring extended hospital stays followed by continuous outpatient appointments. Patients generally receive a customized care plan, which includes medication management, dietary guidelines, and lifestyle changes to support the new liver's function and delay any recurrence of liver damage. Good success rates of liver transplants for NASH patients are encouraging, although regular monitoring remains critical.
Research continues to provide insights into post-transplant outcomes, indicating that long-term survival rates can be significantly enhanced through tailored post-operative care and lifestyle modifications. Engaging in a multidisciplinary approach, involving dietitians, physical therapists, and mental health professionals, can improve recovery experiences. Many patients find camaraderie and support within peer-based groups, benefiting greatly from shared experiences and encouragement.
Moreover, addressing potential complications such as recurrent NASH, metabolic syndrome, and cardiovascular diseases post-transplant is vital. Patients often need tailored education on managing weight gain and blood sugar levels, emphasizing the importance of integrated care strategies that continue even years post-surgery.
| Aspect | NASH as Transplant Indication | Other Liver Diseases |
|---|---|---|
| Primary Cause | Non-alcoholic fatty liver progresses without timely intervention. | Viral infections, genetic conditions, drug-induced damages, etc. |
| Complications | Higher risk of metabolic syndrome-related complications. | Varies based on underlying cause. |
| Long-Term Management | Patients often require lifestyle adjustments to manage weight and control diabetes. | Specific management plans depending on the liver disease origin. |
| Pre-Transplant Challenges | Difficulty in early detection and may require prompt interventions. | Symptom identification differs widely among various diseases. |
| Psychosocial Considerations | Higher chance of depression and anxiety due to dietary changes and lifestyle modifications. | Depend on the patient’s circumstances and support systems. |
Recent studies indicate survival rates post-transplant are quite promising, with a majority of patients living beyond five years post-operation when following recommended care practices. The exact survival rate can depend on various factors, including the recipient's age, pre-existing health conditions, and adherence to medical follow-ups.
Adopting a liver-friendly lifestyle is crucial, encompassing regular physical activity, a balanced diet, and avoiding alcohol and unnecessary medications. Nutrition plays a pivotal role in recovery; patients are encouraged to work with nutritionists to develop meal plans that support liver health.
While the new liver isn't immune to disease, proper management and follow-ups improve outcomes significantly, reducing recurrence risks. Awareness and proactive lifestyle adjustments are critical to mitigating risks associated with metabolic syndrome and preserving the function of the new organ.
Immunosuppressants are essential for preventing organ rejection; however, they also pose risks of infections and other complications. Educating patients on signs of infections and the importance of adhering to prescribed regimens can foster better outcomes.
Complications can include rejection of the organ, infections, and bile duct issues. Long-term patients also prefer to monitor cardiovascular health closely, as there is an increased risk due to the medications used.
Given the complexities and critical nature of liver transplantation for NASH, a thorough understanding of procedures, possible outcomes, and lifestyle changes post-surgery is imperative for both patients and healthcare providers. The concerted efforts in preemptive care, informed decision-making, and adherence to medical advice post-transplant can significantly enhance the quality of life for NASH patients post-transplantation.
With advances in medicine and continued research into liver disease, the landscape of liver transplantation is evolving. Studies to further understand the pathophysiology of NASH are ongoing, contributing to improved diagnostic tools and treatment protocols. As the medical community gains a deeper understanding of fat metabolism and liver regeneration, targeted therapies may emerge that could potentially stabilize or reverse liver damage without surgical intervention.
Moreover, the integration of innovative technologies, including artificial intelligence in matching donors to recipients, could optimize the process of transplantation, making it more efficient. As the demand for transplantable organs grows, further development of bioengineering could eventually allow for the creation of bioengineered livers, potentially alleviating the organ shortage crisis.
On a population level, public health initiatives to prevent obesity, diabetes, and metabolic syndrome remain crucial. Focusing on education, lifestyle modifications, and screening can help curtail the incidence of NAFLD and NASH at the community level. Programs that encourage a balanced diet, physical activity, and overall wellness have the potential to mitigate the risk of these liver diseases significantly.
As these programs take shape, collaboration across clinical, educational, and community sectors will be vital for success. Left unchecked, the continued rise in NAFLD and NASH cases poses a severe, long-term threat to health systems worldwide, necessitating proactive measures to address the root causes of these conditions.
Liver transplantation remains an indispensable treatment for patients with advanced NASH who have exhausted all other treatment options. Through rigorous evaluations, personalized care, and ongoing support, many individuals can successfully navigate the complexities of their condition toward a more hopeful future. The interplay of effective pre- and post-transplant care, alongside lifestyle changes, can markedly improve health outcomes and enhance the quality of life for individuals battling NASH. As research expands and medical techniques advance, the future looks promising for those facing the challenges presented by this debilitating disease.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
