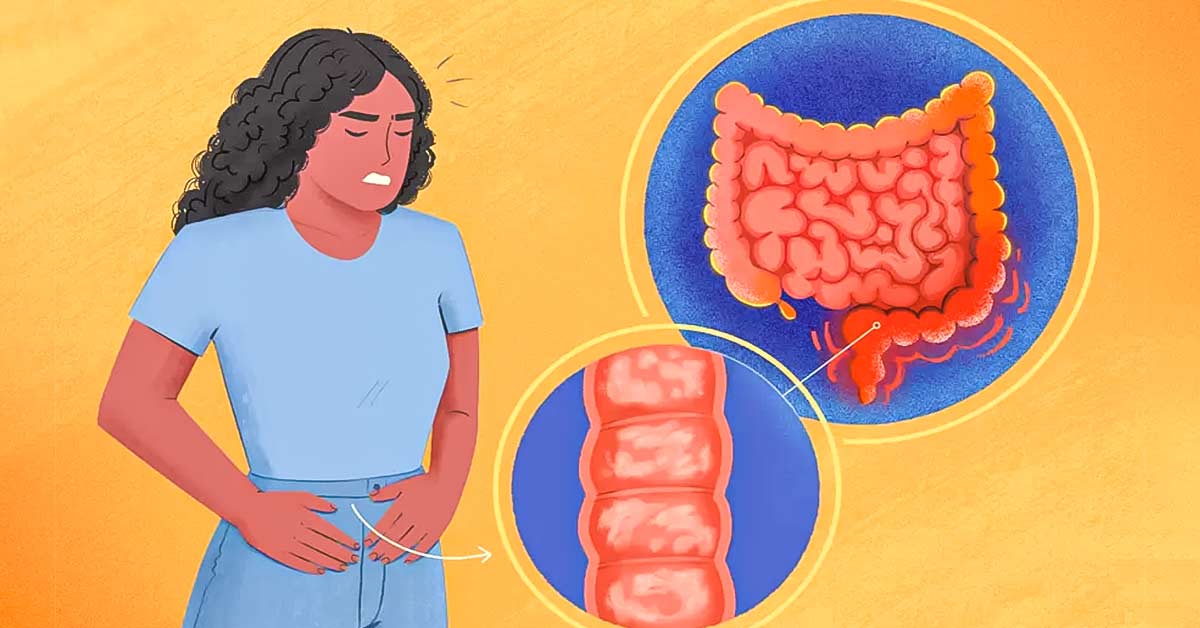
Colitis can significantly impact your life, but early awareness and proper treatment can help manage the condition effectively.

Navigating colitis, an inflammatory condition of the colon, requires early awareness, accurate diagnosis, and effective treatment strategies. This guide provides an overview of colitis, its types, symptoms, potential causes, diagnostic methods, and treatment options to help individuals manage the condition effectively.
Understanding Colitis
Colitis refers to inflammation of the colon (large intestine) and can result from various causes. The most common types include:
- Ulcerative Colitis (UC): A chronic condition characterized by inflammation and ulcers in the lining of the colon and rectum. It typically presents with periods of flare-ups and remission.
- Crohn’s Disease: Although it can affect any part of the gastrointestinal tract, when it affects the colon, it can cause similar symptoms to ulcerative colitis. It involves deeper layers of the intestinal wall and can lead to complications.
- Infectious Colitis: Caused by bacterial, viral, or parasitic infections. Common pathogens include Clostridium difficile, Salmonella, and E. coli.
- Ischemic Colitis: Occurs when blood flow to the colon is reduced, often due to narrowed or blocked blood vessels.
- Microscopic Colitis: A less common form that includes lymphocytic colitis and collagenous colitis, characterized by chronic diarrhea and inflammation that can only be seen under a microscope.
Symptoms of Colitis
Symptoms can vary depending on the type of colitis but commonly include:
- Abdominal pain and cramping
- Diarrhea (which may be bloody in UC)
- Urgency to have a bowel movement
- Fatigue
- Weight loss
- Fever
- Nausea
Potential Causes and Risk Factors
The exact cause of colitis is often unknown, but several factors may contribute:
- Genetics: Family history of inflammatory bowel disease (IBD) increases risk.
- Immune System: An abnormal immune response may trigger inflammation.
- Infections: Certain infections can lead to colitis.
- Diet: While diet alone doesn’t cause colitis, certain foods may exacerbate symptoms.
- Stress: Emotional stress may worsen symptoms but is not a direct cause.
Diagnosis
Early diagnosis is crucial for effective management. Diagnostic methods may include:
- Medical History and Physical Exam: Discussing symptoms and medical history with a healthcare provider.
- Blood Tests: To check for anemia, infection, and inflammation markers.
- Stool Tests: To identify infections or blood in the stool.
- Imaging Tests: CT scans or MRIs can help visualize the colon.
- Endoscopy: Colonoscopy or sigmoidoscopy allows direct visualization of the colon and collection of tissue samples (biopsies) for further analysis.
Treatment Options
Treatment for colitis depends on the type, severity, and individual patient factors. Options may include:
1. Medications
- Anti-Inflammatory Drugs: Aminosalicylates (e.g., mesalamine) are often the first line of treatment for UC.
- Corticosteroids: Used to reduce inflammation during flare-ups but not recommended for long-term use due to side effects.
- Immunosuppressants: Medications like azathioprine or mercaptopurine help suppress the immune response.
- Biologics: Target specific pathways in the inflammatory process (e.g., infliximab, adalimumab) and are used for moderate to severe cases.
- Antibiotics: For infectious colitis, antibiotics may be prescribed to treat bacterial infections.
2. Lifestyle and Dietary Changes
- Dietary Modifications: Keeping a food diary can help identify trigger foods. A low-fiber diet may be recommended during flare-ups, while a balanced diet rich in nutrients is essential for overall health.
- Hydration: Staying well-hydrated is crucial, especially if experiencing diarrhea.
- Stress Management: Techniques such as mindfulness, yoga, and counseling can help manage stress, which may exacerbate symptoms.
3. Surgery
In severe cases of ulcerative colitis or complications from Crohn’s disease, surgical options may be considered, including:
- Colectomy: Removal of part or all of the colon. In UC, this may involve creating an ileal pouch to allow for normal bowel function.
- Strictureplasty: Widening narrowed sections of the intestine in Crohn’s disease.
Monitoring and Follow-Up
Regular follow-up with a healthcare provider is essential for managing colitis effectively. Monitoring may include:
- Regular colonoscopies to assess inflammation and screen for colorectal cancer, especially in long-standing UC.
- Blood tests to monitor for anemia and inflammation.
- Adjustments to treatment plans based on symptoms and disease progression.
Conclusion
Early awareness and proactive management of colitis can significantly improve quality of life and reduce complications. If you experience symptoms suggestive of colitis, it is essential to seek medical advice promptly. Collaborating with healthcare professionals to develop a personalized treatment plan, making lifestyle adjustments, and staying informed about the condition can empower individuals to navigate colitis effectively.