Preventative HIV drugs, known as Pre-exposure Prophylaxis (PrEP), represent a groundbreaking approach in the fight against HIV/AIDS. These medications are designed to prevent HIV infection in high-risk individuals by maintaining sufficient levels of antiretroviral drugs in the bloodstream. Understanding the mechanisms, accessibility, and efficacy of these drugs is vital to leveraging their full potential in public health strategies worldwide.

Preventative HIV drugs, often referred to as Pre-exposure Prophylaxis (PrEP), have emerged as a pivotal tool in the global effort to combat HIV/AIDS. Their primary function is to prevent HIV infection in individuals who are at significant risk. By taking a daily pill that contains specific antiretroviral medicines, individuals can significantly reduce their chance of contracting HIV, offering a crucial layer of protection where other preventive measures might fall short. The rise of PrEP has been nothing short of revolutionary in the fight against HIV, ushering in a new era in which preventing HIV is not only possible but also achievable for at-risk populations.
PrEP works by maintaining a constant level of antiretroviral drugs in the bloodstream. These medications, typically composed of a combination of tenofovir and emtricitabine, inhibit the virus's ability to replicate if an exposure occurs. This process minimizes the chance of the virus establishing a successful infection, making it a highly effective preventive measure when taken consistently and as prescribed. By disrupting the virus's life cycle, PrEP provides a robust defensive mechanism, essentially creating a fortress around one's immune system that prevents the intrusion of HIV. Understanding the pharmacological underpinnings of PrEP is essential not just for those at risk, but also for healthcare providers who prescribe it and public health officials who advocate for its use.
The true effectiveness of preventative HIV drugs is not solely based on biological mechanisms but also on their accessibility and implementation. Ensuring that PrEP is available to those who need it very involves overcoming barriers related to cost, availability, and awareness. Many regions worldwide face challenges addressing the stigma associated with taking PrEP, which can deter individuals from seeking this vital preventive treatment. In various communities, misinformation about PrEP and fear of being judged may lead people to avoid speaking with healthcare providers about it. Comprehensive educational campaigns are necessary to dispel myths surrounding PrEP, helping individuals to better understand its benefits and significance. Furthermore, efforts to integrate PrEP into broader sexual health and wellness programs can also enhance accessibility.
| Drug Name | Components | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Truvada | Tenofovir and Emtricitabine | Up to 99% when taken daily | Nausea, kidney problems |
| Descovy | Tenofovir alafenamide and Emtricitabine | Similar to Truvada | Diarrhea, headache |
| Apretude | Cabotegravir | Up to 90% with injection every two months | Injection site reactions, headache |
In recent years, the landscape of PrEP has continued to evolve with the introduction of newer options such as injectable PrEP. Unlike oral PrEP, which requires daily adherence, Apretude is injected once every two months, offering a potentially more convenient alternative for individuals who struggle with daily medication routines. This innovation is particularly appealing for those who may find the daily pill regimen challenging due to lifestyle factors, thereby broadening the scope of those who can benefit from HIV prevention strategies.
Implementing a comprehensive PrEP program involves addressing several challenges, including education and awareness, affordable pricing, and ensuring consistent access. Effective programs often combine these medications with routine health assessments and continuous education to help potential users understand the importance of regular administration and follow-up care. One of the key challenges in PrEP implementation is the cost of medication and associated healthcare services. Many individuals may not have insurance plans that cover the necessary testing or consultations, which can hinder their ability to access PrEP. In some regions, organizations are working to create assistance programs, reducing financial barriers and making PrEP more affordable and accessible. Furthermore, providing education to healthcare providers as well as potential users can lead to enhanced outreach efforts, ensuring that more individuals are aware of their options.
Healthcare providers play a crucial role in the successful implementation of PrEP programs. By offering proactive counseling and creating a supportive environment free from judgment, they encourage more individuals to consider PrEP as a viable option. Additionally, providers can help monitor adherence, efficacy, and any side effects, ensuring that users receive the maximum benefits of the medication. Building trust between healthcare professionals and individuals seeking PrEP is essential. When patients feel comfortable discussing their health concerns openly, they are more likely to adhere to their prescribed regimen and report any side effects. Training providers to approach conversations about sexual health, including topics like PrEP, in a compassionate manner can dramatically increase the uptake of this critical preventive therapy.
Community engagement is another vital aspect of enhancing PrEP's accessibility. Many individuals at high risk for HIV may feel more comfortable seeking information and care within community settings rather than through traditional healthcare facilities. Innovative approaches, such as mobile health clinics, can bring screening and education directly to at-risk populations. Additionally, peer educators can offer relatable insights and support, bridging the gap between medical advice and personal experience. Community-based organizations often serve as accessible points of contact for individuals who need assistance navigating the healthcare system. These entities should be funded and supported to make an impact in public health by creating focused interventions that resonate with the unique needs and circumstances of their communities.
The stigma associated with HIV continues to pose a significant challenge to PrEP uptake. Misconceptions about those who take PrEP can lead to fear and discrimination, preventing individuals from seeking the medication or engaging in discussions about their sexual health. Public health campaigns aimed at normalizing PrEP and promoting it as a standard preventive measure can help dissipate these stigmas. Education must also address the broader context of sexual health, recognizing that HIV prevention is an essential part of overall wellness. By fostering open dialogues about sexual health and normalizing discussions around PrEP in various settings, we can create a more inclusive environment where individuals feel empowered to take proactive steps to protect themselves.
The effectiveness of PrEP has been demonstrated in numerous clinical trials and real-world studies, evidencing its potential in reducing new infections. For instance, a large-scale study conducted in various urban centers showed a 96% reduction in HIV transmission among those who adhered strictly to their PrEP regimen. Other studies have also highlighted the importance of consistent usage; individuals who took PrEP regularly reported significantly fewer new HIV infections compared to those who did not. The accumulation of evidence supporting PrEP's efficacy not only bolsters its acceptance among healthcare providers but also encourages broader public health strategies that integrate it into routine healthcare practices.
As the global population ages, the demographic of individuals seeking PrEP is also changing. Older adults, traditionally underrepresented in conversations about PrEP, are now being recognized as a significant group at risk for HIV. Factors such as increased divorce rates, a growing number of single individuals, and improved health and life expectancy contribute to a desire for sexual activity among older adults. Tailored education and outreach efforts are necessary to ensure that this population understands their risk and the availability of PrEP as a preventive option. Addressing myths about sexual health and aging, alongside providing healthcare consultations tailored for older adults, is essential as we work to ensure that all demographic groups can access the preventive tools they need.
Globally, the adoption of PrEP varies, influenced by local health policies, socio-economic factors, and cultural attitudes towards HIV/AIDS. In some countries, national health systems have successfully integrated PrEP into their public health strategies, establishing frameworks that allow easy access to screening, counseling, and medication. Other regions still grapple with high levels of HIV stigma, limited healthcare infrastructure, and a lack of public awareness. Global health organizations are key players in disseminating information and resources, directing attention to those communities that are most in need of comprehensive HIV prevention strategies. As international collaboration continues to develop, best practices can be shared and adapted across different contexts, potentially smoothing the path for PrEP accessibility worldwide.
The future of HIV prevention will undoubtedly continue to evolve, incorporating advances in biomedical research, novel treatment approaches, and an increased emphasis on community involvement in health initiatives. As more individuals engage with their health and explore options like PrEP, we can anticipate a decline in new infections. The expansion of telehealth services and mobile health apps could facilitate greater access to information and care, breaking down barriers for at-risk populations. Additionally, vaccine development efforts must also continue to be a focus, as the ultimate goal remains to eliminate the HIV epidemic globally. Research into long-acting formulations, oral medications, and alternative routes of administration will likely shape the landscape of HIV prevention in the coming years.
The success of preventative HIV drugs such as PrEP hinges on more than just their biological efficacy. Their potential is unlocked through comprehensive healthcare strategies that prioritize education, accessibility, and ongoing support. By fostering a global culture of preventive healthcare, these drugs can serve as a cornerstone in the effort to substantially reduce new HIV infections worldwide. Moreover, continuous advocacy, research, and collaboration between various stakeholders—including public health officials, healthcare providers, community organizations, and individuals—will be crucial in making every effort to minimize the transmission of HIV and protect the health of vulnerable populations. As we strive toward the end of the AIDS epidemic, embracing innovations in treatment, enhancing education, and dismantling stigma will drive us closer to a future free from HIV.
Explore the Tranquil Bliss of Idyllic Rural Retreats

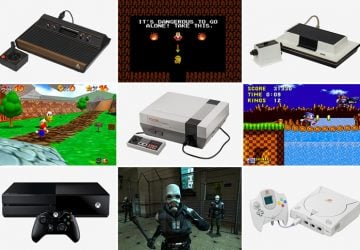
Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!
Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
