This guide delves into the complexities of eczema, focusing on atopic dermatitis, its primary form. Eczema encompasses various skin conditions characterized by inflammation. Atopic dermatitis, prevalent in children but also affecting adults, presents challenges due to its chronic nature. This article offers an expert analysis of symptoms, causes, and treatment options available for managing this condition effectively.
Eczema, commonly misidentified due to its symptomatic similarity to other skin conditions, is a complex disorder impacting a significant portion of the global population. Central to this condition is atopic dermatitis, a chronic form of eczema primarily affecting children but often persisting into adulthood. Its prevalence has steadily increased over the years, with studies indicating that it affects approximately 10-20% of children and about 1-3% of adults worldwide. Managing this condition requires a thorough understanding of its symptoms, triggers, and available treatments. The lifelong journey of dealing with eczema can pose challenges not only physically due to the visible skin changes but also emotionally due to the associated stigma and psychological impacts.
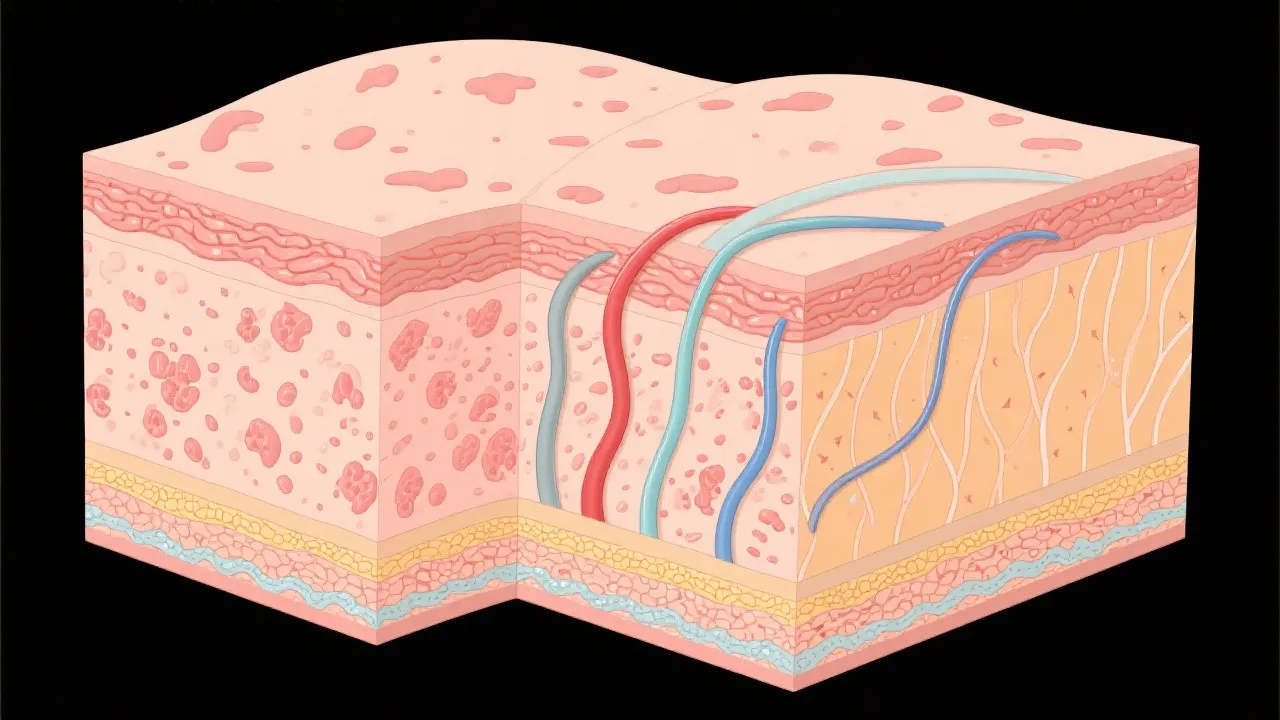
Atopic dermatitis is distinguished by its chronic relapsing nature, characterized by patches of red, itchy, and inflamed skin. While its exact cause remains elusive, a combination of genetic predisposition, environmental influences, and immune system dysfunction contributes to its manifestation. Research suggests that individuals with atopic dermatitis often have a faulty skin barrier, making them more susceptible to irritants and allergens. Patients experience flares that can vary considerably in frequency and intensity, influenced by seasonal changes, stress levels, and lifestyle choices. The emotional toll of dealing with an unpredictable condition like atopic dermatitis can lead to anxiety, depression, and social withdrawal.
Recognizing the symptoms of atopic dermatitis is crucial for early intervention. Common signs include:
Moreover, triggers range from allergens like pollen and dust mites to irritants such as soaps and fragrances, and even environmental factors like stress and climate fluctuations. Weather changes have been noted to exacerbate the condition; for instance, dry winter air can lead to increased dryness and irritation, while humidity can worsen the growth of mold and dust mites. In this context, understanding individual triggers is paramount as it empowers the patient to minimize exposure and manage their condition more effectively.
| Symptom | Description |
|---|---|
| Itching | Persistent, often severe itching that can affect sleep and quality of life. |
| Skin patches | Red, inflamed patches that may become scaly and generally appear in characteristic locations. |
| Skin thickening | Thickened and leather-like skin as a result of chronic scratching. |
| Weeping lesions | Sores that ooze fluid and may become crusty, often indicating a secondary bacterial infection. |
| Dark patches of skin | Skin may also appear darkened in areas that have been frequently scratched or inflamed. |
| Dry skin | Skin feels tight and dry, which can worsen itching and irritation. |
An accurate diagnosis requires a comprehensive examination by a dermatologist. This involves detailed patient history and a physical skin examination to understand the extent and pattern of the skin involvement. In diagnosing atopic dermatitis, it is also essential to differentiate it from other skin conditions such as psoriasis, contact dermatitis, and seborrheic dermatitis, which can have overlapping symptoms.
Moreover, understanding the nuances between eczema types enables tailored treatment plans and effective symptom management. A diagnosis can also include patch testing to identify potential allergens contributing to skin irritation. This process often provides insights that assist both the patient and the physician in managing triggers more effectively. Also, it’s worth noting that some patients can have food triggers that aggravate their condition, which may require consultations with an allergist or dietitian to evaluate dietary restrictions.
Effective management of atopic dermatitis extends beyond skincare. It encompasses lifestyle modifications, environmental adjustments, and psychological support to enhance overall wellbeing. Treatment options include:
Furthermore, lifestyle modifications play a crucial role in management strategies. For instance, developing a daily skincare routine that focuses on gentle cleansing and consistent use of emollients can vastly improve skin barrier function. Additionally, strategies for stress management such as mindfulness, meditation, and cognitive behavioral therapy can combat the emotional challenges posed by chronic skin conditions.
In addition to conventional treatments, many patients explore complementary approaches to manage their skin condition effectively. These can include:
It's crucial to approach these complementary methods as adjuncts to conventional treatment rather than replacements. Each patient's experience with eczema is unique, and what works for one individual may not necessarily work for another.
Q: Can atopic dermatitis be cured?
A: While there is no cure, effective management and treatment can significantly reduce symptoms and improve quality of life. With proper adherence to a treatment plan, many individuals experience long periods of remission.
Q: What lifestyle changes can aid in managing eczema?
A: Identifying and avoiding triggers, maintaining a regular skincare routine, and managing stress levels can alleviate symptoms. Additional lifestyle adjustments may include wearing breathable fabrics, avoiding hot water during showers, and using mild soaps.
Q: Are there any natural remedies effective for atopic dermatitis?
A: Natural remedies like coconut oil and oatmeal baths may provide relief, but should be used in conjunction with professional medical advice. Always discuss with your dermatology provider before trying new treatments.
Q: Do environmental factors play a role in eczema symptoms?
A: Yes, environmental factors such as humidity, temperature, tobacco smoke, and exposure to microbes can significantly influence symptom severity. Understanding individual sensitivities can play an essential role in management.
Q: How can I support a child with atopic dermatitis?
A: Supporting a child with this condition involves education, empathy, and creating an environment that minimizes triggers. Helping them maintain a skincare routine, encouraging them to express their feelings about their skin, and ensuring they wear comfortable clothing can be beneficial.
Managing eczema, particularly atopic dermatitis, involves a multifactorial approach, integrating medical treatments with lifestyle modifications and emotional support. Patients must educate themselves about their condition, as understanding its etiology and symptoms plays a crucial role in successful management. Open communication with healthcare providers allows for the development of a personalized, adaptable treatment plan that addresses the unique challenges presented by this pervasive skin disorder. As research continues to develop new treatments and improve understanding of this condition, there is hope for better, more effective management strategies for those affected by atopic dermatitis.
Given the impact of atopic dermatitis on quality of life, ongoing research is focused on optimizing existing treatments and exploring novel therapies. Advances in genetics have provided insight into specific genetic markers associated with atopic dermatitis. Understanding these genetic aspects can lead to personalized medicine approaches, where treatment is tailored based on an individual's genetic profile.
Furthermore, studies are investigating the microbiome's role in skin health. It is hypothesized that imbalances in skin microbiota may play a part in eczema pathogenesis, potentially leading to probiotics or other microbiome-modulating therapies as new avenues for treatment.
Researchers are also looking into the long-term effects of early intervention and the use of biologics. The potential impact of early initiation of systemic therapies in children, particularly those with severe disease, is under investigation. This could change the landscape of atopic dermatitis management significantly.
As understanding of atopic dermatitis evolves, collaboration between researchers, dermatologists, and the patient community remains essential to drive advancements in combating this chronic skin condition. By continuing to bridge the gap between scientific research and practical application, we strive to enhance the quality of life for those living with eczema and atopic dermatitis.
Many people find that sharing their experiences with others who understand the challenges of living with eczema can be immensely beneficial. Support groups, whether in-person or online, provide platforms for patients to share stories, seek advice, and foster a sense of community. Connecting with others can reduce feelings of isolation, provide new coping strategies, and bolster emotional support.
Furthermore, personal narratives can also be a powerful tool for raising awareness. Individuals can advocate for better understanding and resources for eczema, both in their communities and on social media platforms. This advocacy can often lead to enhanced support and recognition from healthcare systems and society as a whole, emphasizing the need to view skin conditions not only through a medical lens but also through a lens of emotional and social well-being.
Sharing experiences not only helps others find solace in their journey but also encourages a broader discussion about the complexity of eczema, the embodied experiences of individuals, and the necessity for compassionate care. By working together, patients can help promote a more profound understanding of eczema and atopic dermatitis, ultimately driving progress toward better treatments and outcomes for all.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
