The article investigates the intertwined relationship between obesity and Non-Alcoholic Fatty Liver Disease (NAFLD). It delves into how obesity contributes to the prevalence and severity of NAFLD. Furthermore, it assesses the impact of lifestyle, genetic predispositions, and treatment options. As obesity rates climb globally, understanding its relationship with NAFLD becomes increasingly urgent for effective medical intervention and policy-making.
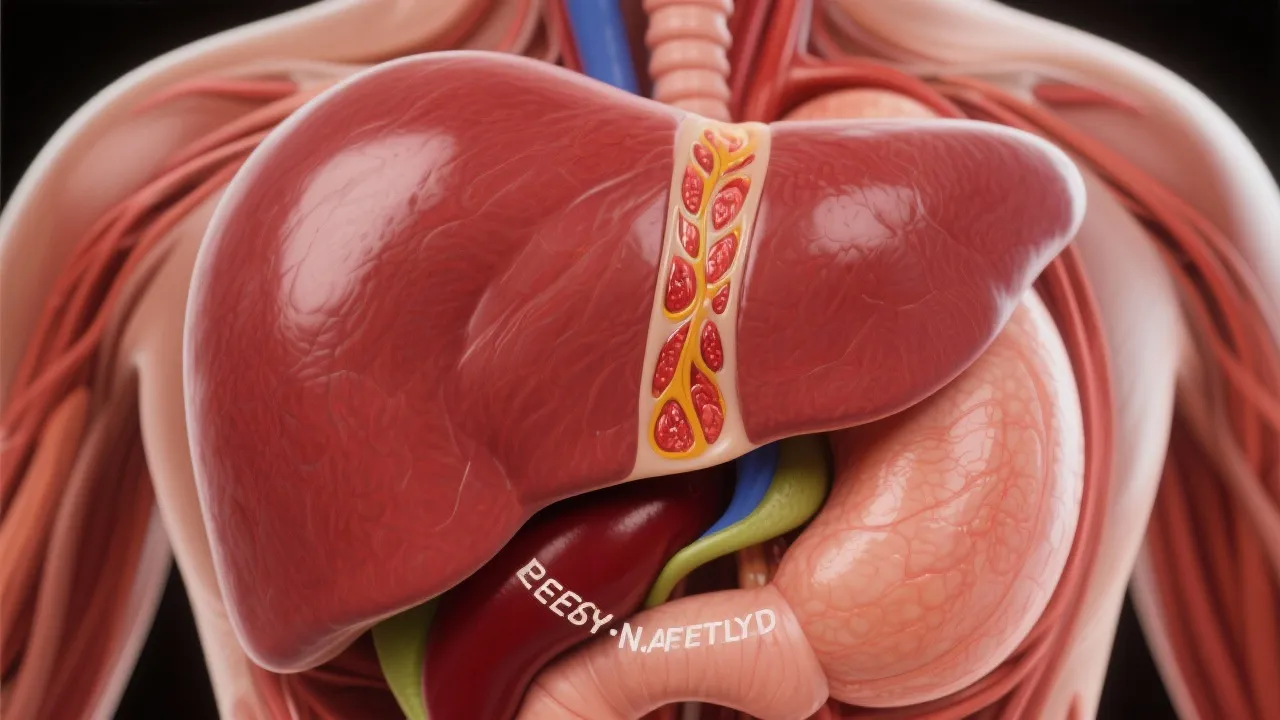
In recent decades, the prevalence of obesity has risen alarmingly worldwide, coinciding with a surge in Non-Alcoholic Fatty Liver Disease (NAFLD). NAFLD is a major public health concern characterized by the accumulation of fat in liver cells, which is not caused by excessive alcohol intake. Understanding the intricate relationship between obesity and NAFLD is critical, particularly given the progressive nature of NAFLD, which can lead to severe liver conditions such as cirrhosis and hepatocellular carcinoma. The World Health Organization (WHO) has recognized obesity as a global epidemic, with millions of people affected, leading to severe health complications. The alarming statistics regarding obesity and its association with NAFLD have prompted researchers and healthcare professionals to investigate this connection further, revealing complex interactions between genetic, environmental, and lifestyle factors.
Obesity is one of the very significant risk factors for NAFLD, accounting for an estimated 80-90% of NAFLD cases. Excess body fat changes metabolic profiles, promoting insulin resistance, a key player in hepatic fat accumulation. Furthermore, obesity-related inflammation contributes to liver damage and fibrosis. In addition to the visceral fat surrounding organs, subcutaneous fat also plays a contributing role in metabolic dysfunction. Studies show that the type and distribution of body fat can influence the severity of liver disease. This connection is primarily mediated through various hormonal and biochemical pathways, whereby excess adipose tissue releases free fatty acids and inflammatory cytokines into the bloodstream, further exacerbating liver injury. Understanding these links highlights the need for targeted interventions to tackle both obesity and subsequent liver complications.
The pathogenesis of NAFLD in obesity involves multiple metabolic pathways. Insulin resistance boosts lipolysis, leading to increased affordable fatty acid delivery to the liver. This exacerbates hepatic fat accumulation while also impeding very low-density lipoprotein (VLDL) secretion. Insulin also plays an essential role in glucose metabolism, and elevated insulin levels can lead to a decrease in the activity of enzymes responsible for fatty acid oxidation in liver cells. Notably, the interaction between elevated insulin levels and increased fatty acid production creates a vicious cycle that accelerates the progression of NAFLD. Additionally, an imbalance in adipokines, hormones produced by adipose tissue, furthers liver inflammation and damage. Leptin, an adipokine that is elevated in obesity, is known to promote inflammation and disrupt the balance of normal metabolism in the liver.
According to a study published in the Journal of Hepatology, obese individuals have a sevenfold increased likelihood of developing NAFLD compared to those with a normal weight. This correlation is further supported by extensive epidemiological studies, which reveal that other conditions associated with obesity, such as metabolic syndrome, significantly heighten the risk for NAFLD. Further research revealed that approximately 25-30% of those with NAFLD progress to non-alcoholic steatohepatitis (NASH), a more severe form that could lead to liver fibrosis and cirrhosis. To paint a clearer picture, the prevalence of NAFLD among individuals with type 2 diabetes can be as high as 70%. These findings emphasize the importance of early detection and intervention for individuals at a higher risk of developing NAFLD due to obesity and metabolic syndrome.
Currently, there are no FDA-approved medications specifically for NAFLD. The cornerstone of managing NAFLD is lifestyle modification, focusing on weight loss through diet, exercise, and managing underlying conditions such as type 2 diabetes and dyslipidemia. A study in the New England Journal of Medicine highlighted that a 7-10% weight loss could significantly improve liver histology. Additionally, engaging patients in regular exercise has shown promising results in enhancing liver health markers, demonstrating improvements in insulin sensitivity and reductions in fat accumulation in the liver. Nutritional interventions emphasizing a balanced diet rich in fruits, vegetables, whole grains, and healthy fats are of paramount importance. Moreover, the implementation of behavioral strategies—such as cognitive-behavioral therapy and structured support groups—can motivate and sustain lifestyle changes for long-term benefits.
Recent advancements in the understanding of molecular mechanisms offer hope for the development of targeted therapies. Genetic studies aim to identify individuals susceptible to NAFLD due to specific genetic markers, thereby allowing personalized medicine approaches. Research into the microbiome has also emerged as a fascinating area of study, revealing that gut health might significantly influence liver health and the development of NAFLD. Ongoing investigations are delving into the role of dietary patterns, microbial diversity, and the impact of probiotics and prebiotics in alleviating liver fat. Furthermore, the exploration of pharmacological agents targeting the underlying pathophysiology of NAFLD, such as agents focusing on insulin sensitivity and lipid metabolism, presents an exciting frontier in the quest to find effective treatments.
| Factor | Obesity Impact on NAFLD |
|---|---|
| Insulin Resistance | Promotes hepatic steatosis by increasing lipolysis and FFA delivery to the liver. This condition diminishes the liver's ability to metabolize fats efficiently. |
| Inflammation | Adipose tissue dysregulation leads to inflammatory cytokines affecting liver health, which may result in fibrosis and escalation towards NASH. |
| Genetic Predisposition | Certain genetic markers can increase NAFLD risk, highlighting a potential basis for tailored preventive strategies based on genetic profiling. |
| Dietary Habits | Poor dietary choices, such as high sugar and fat intake, can exacerbate obesity and accelerate liver damage in individuals prone to NAFLD. |
| Physical Activity | Lack of physical activity contributes to obesity and worsens NAFLD by impairing the metabolism of fats and sugars, thus emphasizing the need for regular exercise. |
Q: How closely related are obesity and NAFLD?
A: Obesity is considered a primary risk factor for NAFLD, significantly elevating the likelihood of developing the condition. The association is complex and multifactorial, involving metabolic, inflammatory, and lifestyle factors.
Q: Can NAFLD be reversed through weight loss?
A: Yes, research indicates that moderate weight loss can result in substantial improvements in liver health in NAFLD patients. A consistent lifestyle intervention strategy is crucial for reversing the disease's progression.
Q: Are there effective medical treatments for NAFLD?
A: Currently, there are no specific FDA-approved drugs for NAFLD, making lifestyle changes vital for disease management. Clinical trials are ongoing to explore potential pharmacotherapies, but lifestyle modification remains the mainstay of treatment.
Q: What role does diet play in managing NAFLD?
A: A well-balanced diet is integral to managing NAFLD. Emphasizing whole foods, minimizing sugar and unhealthy fats, and maintaining an appropriate caloric deficit can aid in liver health restoration.
Q: How prevalent is NAFLD among different populations?
A: The prevalence of NAFLD varies by population demographics, with higher rates observed among individuals with obesity, type 2 diabetes, and specific ethnic groups such as Hispanic and Asian communities.
In conclusion, addressing the global obesity epidemic is paramount in managing and reducing the burden of NAFLD. While lifestyle interventions currently form the core of treatment strategies, ongoing research into the pathophysiology of obesity-related NAFLD holds the promise of novel therapeutic approaches. Effective public health policies promoting healthy lifestyle behaviors are essential in tackling these intertwined health challenges. Furthermore, public awareness campaigns aimed at educating individuals on the risks associated with obesity and NAFLD can help catalyze change at the community level. The fight against obesity and NAFLD is multifaceted, requiring a concerted effort from healthcare providers, patients, and society at large.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
